Defining What “Quality Care” Means for Otolaryngology: Call for Measures
Find out how to submit topics for consideration in the development of new quality measures.

We encourage measure concepts have a strong evidence-base and focus on those conditions or outcomes of highest importance to patients and healthcare providers. Measures may focus on the following:
- Prevention
- Management of acute and chronic conditions
- Appropriate use
- Clinical and patient-reported outcomes
While not all concepts can move forward, the measure development team considers all measure suggestions for development or expansion or revision of an existing quality measure. When concepts are evaluated for development, the submitters are encouraged to consider the following:
Feasibility/data element requirements
Concepts are evaluated to determine the consistent availability of data elements within a measure. For example, over-the-counter medications can be inconsistently documented in various locations within the medical record. However, assessment of a prescribed medication has proven to be more consistently documented. For concepts not codified, it can be captured by keywords and phrases, but to minimize clinician burden and improve reliability, codified concepts are preferred.
Unintended consequences
While quality measures are developed to promote quality care, they also can unveil unintended consequences. This can occur with all measures but is more common in measures that address appropriate use of healthcare resources. For example, a measure discouraging oncology patients from receiving oxygen therapy.
Duplicative
If a similar concept is submitted to an existing measure within our measure repository, a new measure would not be developed but would be considered for a revision of the current quality measure to expand the patient population.
Gaps and variation in care
Documented evidence of deviation (or observed patterns of deviation) in care from established norms or standards of care; gaps in care may be manifested by underuse, overuse, or misuse of health services. Preliminary data, if available, will be considered. If data shows most of our participants meet the metric, it will not move forward as there would be little room for improvement. This also aligns with requirements to be approved as a Qualified Clinical Data Registry (QCDR) measure.
Evidence base
Sufficient confidence in existing evidence to support measure development; evidence should ideally come from published research, such as guidelines, systematic reviews, or clinical consensus statements, but other observational evidence may suffice.
For more information and to submit measurement topics and concepts, login to the Call for Clinical Quality Measure Development Topics page.
We accept concepts on a rolling basis. To be considered for the subsequent performance year, we require the concept be submitted by February 28. This allows internal vetting, discussions with CMS, approval processes, and development (including face validity testing) of the measure prior to the September 1 self-nomination deadline.
Visit the AAO-HNSF Quality Measures page for more information about current endorsed quality measures and the quality measures development process.
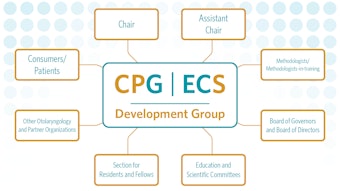
Additional Resources: The Anatomy of a Measure
How are AAO-HNSF clinical quality measures (CQMs) calculated? CQMs are used to assess how well healthcare providers adhere to evidence-based clinical recommendations to achieve desired outcomes. This video identifies each of the measure elements and demonstrates how these are used to calculate the AAO-HNSF CQMs.