How Migraine Modulates Tinnitus
It has been found that migraine is more common in patients with tinnitus and subjective hearing loss.
Mehdi Abouzari, MD, PhD, and Hamid R. Djalilian, MD, AAO-HNS Hearing Committee

In the United States, a cross-sectional study discovered that approximately 2.5 million young people aged 12 to 19 have encountered one or more instances of tinnitus.3 Among this demographic, around 1.6 million individuals experience chronic tinnitus.3 The emotional and psychological impact on those with tinnitus is a potential issue, as untreated tinnitus could lead to indications of depression and anxiety. However, it is worth noting that individuals already suffering from depression and anxiety might somaticize their symptoms through tinnitus and blame their tinnitus as the source of their problems. Treatment of the underlying anxiety or depression by psychiatry and psychology helps those patients to make their tinnitus less annoying.
Fluctuating tinnitus in some patients can be a migraine or central sensitivity disorder phenomenon. In these patients, the activation of the migraine process may lead to a temporary change in hearing and thus increase in tinnitus through the activation of the trigeminal ganglion and altered blood flow to the inner ear.4 This altered blood flow can lead to a decrease in hearing and thus tinnitus.
Another link between migraine/central sensitivity disorder and tinnitus is the increased attention to tinnitus during migraine. We have found that the triggers of the increased loudness of tinnitus in these patients are the same as those seen in migraine headache patients (i.e., stress, poor sleep, diet, etc.). We will explain this link between fluctuating or loud tinnitus and migraine in more detail from an epidemiological and mechanistic perspectives. Finally, we will explain the potential for migraine treatments to be considered in the management and treatment of significantly bothersome and fluctuating tinnitus.
Migraine Is More Common in Patients with Tinnitus and Vice Versa
It has been found that migraine is more common in patients with tinnitus and subjective hearing loss. In an analysis of the National Health and Nutrition Examination Survey (NHANES) database, we found that among 12,962 patients with tinnitus or subjective hearing loss, migraine was reported in 36.6% and 24.5% respectively.5 We also found that patients with tinnitus were more likely to have migraine, and that patients with migraine were more likely to have subjective hearing loss and tinnitus.5 Furthermore, the Hwang, et al. cohort study revealed that among 1,056 patients with migraine, 61.5% of patients with vestibular migraine experienced auditory symptoms with tinnitus being the most common symptom.6 These findings suggest that there may be a mechanistic link between migraine and enhanced attention to the dysregulation of the central auditory pathway in a subpopulation of tinnitus.
How Does Migraine Cause Enhanced Tinnitus Perception?
The primary theory explaining the underlying mechanisms of migraine revolves around the activation of peripheral and central trigemino-vascular system (Figure 1). The trigemino-vascular neurons synapse with blood vessels and release specific neuropeptides and become activated after spreading cortical depression. These neurons secrete cytokines like calcitonin gene-related peptide (CGRP), substance P, neurokinin A, and pituitary adenylate cyclase-activating polypeptide.7,8 This abnormal release of molecules leads to processes such as vasodilation, plasma leakage, and mast cell degranulation. Consequently, this sequence of events creates a persistent state of neuroinflammation in the meninges.9,10 Furthermore, there is a connection between the inner ear (specifically the vestibule and cochlea) and the ophthalmic branch (CN V1) of the trigeminal nerve. Heavy CN V1 innervation of the spiral modiolar artery and the stria vascularis have been found in animal studies.11 Stimulation of CN V1, as would be seen in an active migraine process, was found to cause fluid extravasation in the cochlea within 60 minutes.12 This fluid extravasation in the cochlea, which is likely due to trigeminal nerve inflammation and vasodilation in the inner ear's circulation, contributes to changes in the cochlea that are associated with the migraine state.13 These neurovascular changes potentially provide an explanation for various cochleovestibular symptoms seen in migraine, including tinnitus, which can occur with hearing disturbance. It appears that the trigeminal innervation of the cochlear vasculature may cause a change in hearing in a migraine activation, which can lead to tinnitus development.
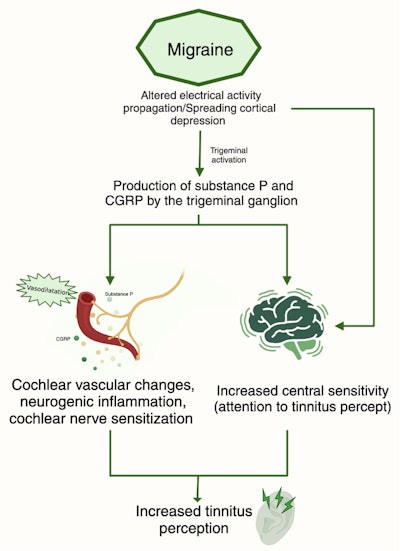 Figure 1. Schematic diagram of the migraine mechanisms leading to tinnitus perception.
Figure 1. Schematic diagram of the migraine mechanisms leading to tinnitus perception.
Migraine has recently been explored as a possible cause of inner ear disorders including Ménière’s disease, vertigo, sensorineural hearing loss, and potentially tinnitus.14-16 Specifically, two variants of migraine—vestibular migraine and cochlear migraine—demonstrate connections with dysfunction within the inner ear. To comprehend the relationship between both forms of migraine and tinnitus, it is essential to delve into the underlying mechanism that ties them together. Tinnitus arises in instances of impairment within the peripheral auditory system.17 When hair cells in the basal turn of the cochlea experience functional deterioration, it leads to reduced lateral inhibition at the central level. Consequently, this triggers a reorganization of the tonotopic map in the auditory cortex. This reorganization, in turn, causes spontaneous neuronal firing in the cortex, which the patient perceives as tinnitus.18 The role of cochlear dysfunction in migraine mediated by the activity of outer hair cells has also been noted in otoacoustic emission (OAE) testing in migraine patients. A study revealed that the amplitude of OAEs was notably lower in individuals with migraine compared to controls.19 Additionally, the suppression of transiently evoked OAEs by contralateral sound stimulation, typically observed in controls, was absent in migraine patients.19 This absence of suppression could potentially contribute to the mechanism behind hyperacusis experienced by migraine sufferers.
Migraine and Tinnitus Have Common Triggers
Drawing from our experience in treating patients with tinnitus, we have observed common triggers shared between tinnitus and migraine (Table 1). These triggers encompass factors such as sleep disruptions, stress, dietary patterns, and changes in weather conditions. Notably, foods rich in sodium, often containing additives like glutamate or byproducts of protein breakdown such as tyramine, frequently act as triggers for migraine headaches.20 The consumption of sodium-rich foods, leading to a state of relative dehydration, in conjunction with dehydration itself, can spark migraine headaches. Tyramine, also present in fermented items, alcoholic beverages like wine and beer, and aged cheeses, contributes to this effect. It is worth mentioning that a low-sodium diet is frequently recommended as a primary approach for addressing inner ear symptoms. This dietary adjustment is believed to elevate plasma aldosterone levels, influencing the regulation of endolymph within the inner ear.20 In our observation of patients who report improvement with a low sodium diet, we have found that most of the food items they eliminated were glutamate- or tyramine-rich foods. In addition, we have found that patients who link high sodium with increased inner ear symptoms do not experience exacerbation if increased water intake accompanies the higher sodium intake, when glutamate and tyramine are avoided. Therefore, adequate hydration and the unintended reduction in glutamate and tyramine likely causes the benefit rather than the sodium reduction.
Table 1. Summary of dietary and physiologic migraine triggers.

Additionally, caffeine overuse or withdrawal has been identified as a trigger of migraine. Caffeine acts by blocking adenosine receptors, and adenosine is important in modulating neuronal activity, particularly neurotransmitter release. Caffeine, therefore, acts to increase wakefulness and arousal by blocking adenosine receptors, which inhibits GABAergic output to the hypothalamus. We recommend patients slowly wean off caffeine as any caffeine usage can trigger migraine. We have found that fermented alcohols (wine/beer) are the second most common dietary trigger following caffeine. Stress is another well‐understood trigger of tinnitus, as perceived stress has been shown to be the most commonly reported trigger of migraine headaches.21
Meteorological changes such as atmospheric pressure changes have also been proposed as migraine triggers. A retrospective review of 130 patients with vestibular migraine showed 26% of them reported weather changes as being a trigger.22 A prospective study also found a correlation between depressed barometric pressure with headache frequency.23 Barometric data revealed that the frequency of headaches increased significantly just before barometric depression, such as in a typhoon or rainstorm. Some studies, however, have not found a significant correlation between meteorological changes and migraine.24 This may be because only a subpopulation of migraine sufferers is sensitive to weather and atmospheric pressure changes, as we have observed in our clinical practice and in other studies. In the clinic, we often see patients who report that their tinnitus can be triggered by weather changes. This is most commonly observed with low atmospheric pressure, which has been found to be associated with the exacerbation of the Ménière’s disease symptoms including tinnitus.25
Lastly, it is important to note that both migraine and tinnitus can be prompted by exposure to loud sounds. Frequently, patients report a transient amplification in their tinnitus following exposure to loud but nonharmful noises, like those found in restaurants, high-frequency sounds, or ambulance sirens. This temporary escalation in tinnitus perception is likely a result of a momentary increase in migraine-related brain sensitivity triggered by the loud or high-frequency auditory input. While complete avoidance of loud sounds is not always feasible for patients, this phenomenon provides additional support for the hypothesis that controlling the underlying migraine process could potentially lead to improvements in tinnitus.
Tinnitus Treatment: Background
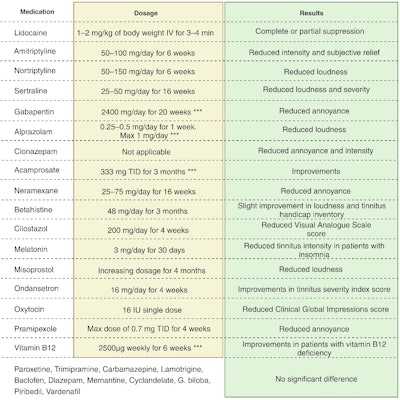
Most tinnitus treatment is focused on symptomatic improvement, decreasing tinnitus intensity and annoyance to the patient. However, there is currently no Food and Drug Administration (FDA)-approved medication specifically for tinnitus treatment. For treatment, most people achieve remission through natural habituation.26 Other forms of therapy include cognitive behavioral therapy (CBT), music or sound therapy, tinnitus retraining therapy, stretching or massaging, and electrical suppression.27 Pharmacotherapy that showed promising results in trials included tricyclic antidepressants and benzodiazepines.28,29 Lidocaine also proved efficacious in treating tinnitus; however, since it can only be administered intravenously, has a short half-life, and has an adverse side effect profile, it cannot be used clinically.30 Many trials testing various pharmacotherapies showed no efficacy when compared to placebos, as detailed in Table 2. Within our clinical practice, we have seen a reduction in the intensity of loud tinnitus among patients who have undergone the migraine treatment regimen and adopted strategies to manage their migraine triggers. It appears that addressing the root cause of migraine substantially diminishes the fluctuations—those periods of pronounced and bothersome loudness—in individuals experiencing tinnitus. It is worth noting that the continuous, subtle level of tinnitus remains unaffected by migraine treatment, as the baseline tinnitus stems from the foundational cochlear damage and central activation. However, loud and fluctuating tinnitus can be reduced through migraine-focused therapies.
Table 2. Studied medications for the treatment of tinnitus.
Non-pharmacological strategies, such as CBT for stress reduction and music therapy commonly used for migraine headaches, have also shown potential for easing tinnitus. A comprehensive analysis pooling odds ratios from various studies demonstrated a significant improvement in clinically meaningful outcomes following CBT treatment and a three-month follow-up in children and adolescents, surpassing the effects of placebo treatment alone.31 In a preliminary study, we reported the efficacy of an eight-week internet-based CBT (iCBT) program, encompassing elements like behavioral coaching, stress and sleep management, meditation and breathing exercises, migraine dietary guidelines, and more, combined with individualized sound therapy incorporating frequency-matched sounds blended with music.32 This combined approach exhibited greater improvement in tinnitus-specific quality of life measures compared to our previous trial involving music and customized sound therapy alone.33
The Migraine Approach to Treating Tinnitus
Otologic migraine describes migraine-induced symptoms impacting the ear, spanning auricular discomfort or pain, cochlear issues such as hearing loss and tinnitus, and vestibular symptoms. In essence, otologic migraine captures the influence of migraine on ear-related symptoms, potentially contributing to the connection between tinnitus and migraine. Furthermore, we adopt a holistic "integrative neurosensory rehabilitation" strategy for managing migraine patients, which involves comprehensive lifestyle adjustments (reducing stress and sleep management), dietary modifications (increased hydration, prevention of hunger, and identification of dietary triggers), and the incorporation of supplements like magnesium and riboflavin, alongside pharmacological interventions when necessary. This systematic approach for addressing tinnitus within the context of migraine is visually depicted in Figure 2. Our findings reveal significant improvement in tinnitus perception among patients with loud, bothersome tinnitus or those experiencing fluctuating tinnitus when addressing the underlying migraine causation. While this regimen does not cure (silence) tinnitus, it substantially reduces its impact. In a recent randomized clinical trial, we evaluated the efficacy of two innovative migraine prophylactic medications versus placebo in treating bothersome or fluctuating tinnitus. The comprehensive results of this clinical trial will be shared in the near future.
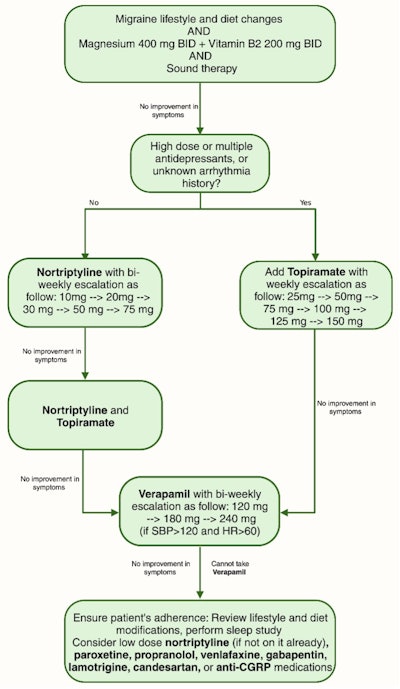 Figure 2. Integrative neurosensory rehabilitation algorithm for treatment of tinnitus.
Figure 2. Integrative neurosensory rehabilitation algorithm for treatment of tinnitus.
Disclosures: Dr. Djalilian is an advisor to and holds equity in NeuroMed Care LLC (telemedicine platform for the medical treatment of tinnitus). He also holds equity in Elinava Technologies (xtinnitus.com, an internet-based cognitive behavioral therapy for tinnitus and beyondtinnitus.com, a sound and music therapy software for tinnitus), Cactus Medical LLC (otitis media diagnosis device), and is an advisor to NXT Biomedical LLC (direct drive hearing aid). Dr. Djalilian also has pending patents related to tinnitus treatment. Dr. Abouzari has no relevant disclosures.
References
- Dietrich S. Earliest historic reference of ‘tinnitus’ is controversial. J Laryngol Otol. 2004;118:487‐488.
- Hamidi S, Sajjadi H, Boroujerdi A, Golshahi B, Djalilian HR. Avicenna's treatise on otology in Medieval Persia. Otol Neurotol. 2008;29:1198‐1203.
- Mahboubi H, Oliaei S, Kiumehr S, Dwabe S, Djalilian HR. The prevalence and characteristics of tinnitus in the youth population of the United States. Laryngoscope. 2013;123:2001‐2008.
- Lee A, Abouzari M, Akbarpour M, Risbud A, Lin HW, Djalilian HR. A proposed association between subjective nonpulsatile tinnitus and migraine. World J Otorhinolaryngol Head Neck Surg. 2023;9:107-114.
- Goshtasbi K, Abouzari M, Risbud A, Mostaghni N, Muhonen EG, Martin E, et al. Tinnitus and subjective hearing loss are more common in migraine: a cross-sectional NHANES analysis. Otol Neurotol. 2021;42:1329-1333.
- Hwang JH, Tsai SJ, Liu TC, Chen YC, Lai JT. Association of tinnitus and other cochlear disorders with a history of migraines. JAMA Otolaryngol Head Neck Surg. 2018;144:712-717.
- Noseda R, Burstein R. Migraine pathophysiology: Anatomy of the trigeminovascular pathway and associated neurological symptoms, cortical spreading depression, sensitization, and modulation of pain. Pain. 2013;154:S44-S53.
- Goadsby PJ, Holland PR, Martins-Oliveira M, Hoffmann J, Schankin C, Akerman S. Pathophysiology of migraine: a disorder of sensory processing. Physiol Rev. 2017;97:553-622.
- Lempert T, Neuhauser H. Migrainous vertigo. Neurol Clin. 2005;23:715-730.
- Ashina M, Hansen JM, Do TP, Melo-Carrillo A, Burstein R, Moskowitz MA. Migraine and the trigeminovascular system-40 years and counting. Lancet Neurol. 2019;18:795-804.
- Vass Z, Shore SE, Nuttall AL, Miller JM. Direct evidence of trigeminal innervation of the cochlear blood vessels. Neuroscience. 1998;84:559‐567.
- Vass Z, Steyger PS, Hordichok AJ, Trune DR, Jancsó G, Nuttall AL. Capsaicin stimulation of the cochlea and electric stimulation of the trigeminal ganglion mediate vascular permeability in cochlear and vertebro-basilar arteries: a potential cause of inner ear dysfunction in headache. Neuroscience. 2001;103:189-201.
- Lin HW, Djalilian HR. The role of migraine in hearing and balance symptoms. JAMA Otolaryngol Head Neck Surg. 2018;144:717-718.
- Frank M, Abouzari M, Djalilian HR. Meniere's disease is a manifestation of migraine. Curr Opin Otolaryngol Head Neck Surg. 2023 Jun 3. doi: 10.1097/MOO.0000000000000908.
- Dash AK, Panda N, Khandelwal G, Lal V, Mann SS. Migraine and audiovestibular dysfunction: is there a correlation. Am J Otolaryngol. 2008;29:295‐299.
- Bayazit Y, Yilmaz M, Mumbuç S, Kanlikama M. Assessment of migraine‐related cochleovestibular symptoms. Rev Laryngol Otol Rhinol (Bord). 2001;122:85‐88.
- Rüttiger L, Singer W, Panford‐Walsh R, et al. The reduced cochlear output and the failure to adapt the central auditory response causes tinnitus in noise exposed rats. PLoS One. 2013;8:e57247.
- Eggermont JJ. Central tinnitus. Auris Nasus Larynx. 2003;30 Suppl:S7‐S12.
- Bolay H, Bayazit Y, Gündüz B, et al. Subclinical dysfunction of cochlea and cochlear efferents in migraine: an otoacoustic emission study. Cephalalgia. 2008;28:309‐317.
- Borkum JM. Migraine triggers and oxidative stress: a narrative review and synthesis. Headache. 2015; 56:12-35.
- Volcy M, Sheftell FD, Tepper SJ, Rapoport AM, Bigal ME. Tinnitus in migraine: an allodynic symptom secondary to abnormal cortical functioning. Headache. 2005; 45:1083‐1087.
- Beh SC, Masrour S, Smith SV, Friedman DI. The spectrum of vestibular migraine: clinical features, triggers, and examination findings. Headache. 2019;59:727‐740.
- Kimoto K, Aiba S, Takashima R, et al. Influence of barometric pressure in patients with migraine headache. Intern Med. 2011;50:1923‐1928.
- Elcik C, Fuhrmann CM, Mercer AE, Davis RE. Relationship between air mass type and emergency department visits for migraine headache across the Triangle region of North Carolina. Int J Biometeorol. 2017;61:2245‐2254.
- Schmidt W, Sarran C, Ronan N, et al. The weather and Ménière's disease: a longitudinal analysis in the UK. Otol Neurotol. 2017;38:225‐233.
- Tyler RS. Neurophysiological models, psychological models, and treatments for tinnitus. In Tinnitus Treatment. Thieme: New York, NY, USA, 2006; pp. 1-22.
- Han BI, Lee HW, Kim TY, Lim JS, Shin KS. Tinnitus: characteristics, causes, mechanisms, and treatments. J Clin Neurol. 2009;5:11-19.
- Dobie RA. A review of randomized clinical trials in tinnitus. Laryngoscope. 1999;109:1202-1211.
- Murai K, Tyler RS, Harker LA, Stouffer JL. Review of pharmacologic treatment of tinnitus. Am J Otol. 1992;13:454-464.
- Sanchez TG, Balbani AP, Bittar RS, Bento RF, Câmara J. Lidocaine test in patients with tinnitus: Rationale of accomplishment and relation to the treatment with carbamazepine. Auris Nasus Larynx. 1999;26:411-417.
- Hesser H, Weise C, Westin VZ, Andersson G. A systematic review and meta‐analysis of randomized controlled trials of cognitive behavioral therapy for tinnitus distress. Clin Psychol Rev. 2011;31:545‐553.
- Abouzari M, Goshtasbi K, Sarna B, et al. Adapting personal therapies using a mobile application for tinnitus rehabilitation: a preliminary study. Ann Otol Rhinol Laryngol. 2021;130:571‐577.
- Mahboubi H, Haidar YM, Kiumehr S, Ziai K, Djalilian HR. Customized versus noncustomized sound therapy for treatment of tinnitus: a randomized crossover clinical trial. Ann Otol Rhinol Laryngol. 2017;126:681-687.