Attack of the Killer….Brisket?
Mammalian Meat Allergy or alpha-gal is an unusual variant of a Type 1 Immunoglobulin E [IgE]-mediated hypersensitivity reaction.
Christine B. Franzese, MD, AAO-HNS Allergy, Asthma, and Immunology Committee

If you find yourself scratching your head wondering what exactly this Mammalian Meat Allergy is or if you have never heard of an allergic reaction to alpha-gal, you’re not alone. In a recent Centers for Disease Control and Prevention (CDC) survey, of 1,500 responding physicians and physician extenders, 42% had never heard of alpha-gal or MMA, and of those who had heard of it, almost half (48%) did not know the correct tests to order to confirm the diagnosis. Of those survey respondents who had heard of MMA, only 5% correctly answered all three questions related to etiology, testing, and patient counseling, with pediatricians scoring the highest.
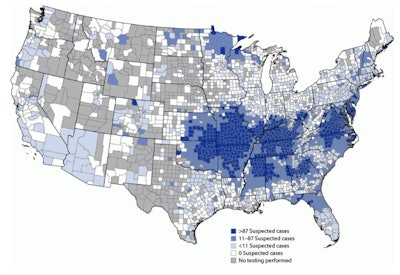 Figure 1. Geographic distribution of suspected alpha-gal syndrome cases* per 1 million population per year — United States, 2017–2022.
Figure 1. Geographic distribution of suspected alpha-gal syndrome cases* per 1 million population per year — United States, 2017–2022.
Centers for Disease Control and Prevention: Thompson JM, Carpenter A, Kersh GJ, Wachs T, Commins SP, Salzer JS. Geographic Distribution of Suspected Alpha-gal Syndrome Cases — United States, January 2017–December 2022. MMWR Morb Mortal Wkly Rep 2023;72:815–820.
The term “alpha-gal” is a shortened version of the name of the sugar molecule responsible for the reaction, galactose-α-1,3-galactose, which is found in most mammals but is not in fish, amphibians, birds, old world apes, or humans. Mammalian Meat Allergy or alpha-gal is an unusual variant of a Type 1 Immunoglobulin E [IgE]-mediated hypersensitivity reaction. Type 1 hypersensitivity reactions mediated by IgE are termed “immediate” hypersensitivity reactions because those reactions typically occur within five to 30 minutes after exposure. However, in the case of alpha-gal, this Type 1 IgE reaction is delayed for several hours after exposure, which can make it challenging to diagnose. Alpha-gal is also not a “fixed” allergy, meaning that ingesting mammalian meat may not always cause a reaction and that the allergy is actually lost over time.
 Image Credit: CW David Chang, MD
Image Credit: CW David Chang, MD
Making the diagnosis of MMA requires symptoms plus positive diagnostic testing. Most commonly MMA presents anywhere from two to 10 hours or possibly longer with hives and was originally termed “midnight urticaria,” as patients with MMA would wake from sleep suffering from acute urticaria. In addition, MMA can also present with angioedema, diarrhea, nausea, vomiting, respiratory symptoms, abdominal pain, and even anaphylaxis. Diagnostic testing includes specific IgE (sIgE) to galactose-α-1,3-galactose but may also include sIgE to pork, beef, and dairy. There is some dispute about what level of sIgE constitutes a positive test, but currently it is considered by many to be positive if antibodies are ≥2 IU/ml or >2% of the total IgE. Others consider any amount to be clinically important, even in asymptomatic patients, as galactose-α-1,3-galactose sensitization has been reported to be a significant risk factor for coronary artery disease.
Once the diagnosis of MMA has been made, patients should be counseled on the avoidance of mammalian meat, not just red meat. Some MMA patients have reactions to glycerin and products derived from mammals, such as cow’s milk or other dairy products. Gelatin-coated medications, medications derived from mammals or containing the alpha-gal oligosaccharide, such as cetuximab, and certain vaccines may also need to be avoided in some MMA patients. MMA is lost over time, so patients need to be counselled in tick precautions to prevent re-sensitization, which may increase the duration of MMA. Wearing long sleeved shirts and pants, using appropriate tick repellant, and full-body surveillance after going outdoors are all important aspects of MMA patient education.
So, before you sit down to a nice, tasty plate of pulled pork, think about any tick bites you’ve had this year and maybe stick with the Hot Chicken?
You’re welcome.
VIDEO: Tiny Tick Bite Can Trigger Dangerous Meat Allergy
References
- Carpenter A, Drexler NA, McCormick DW, et al. Health care provider knowledge regarding Alpha-gal Syndrome — United States, March–May 2022. MMWR Morb Mortal Wkly Rep 2023;72:809–814.
- O'Neil BH, Allen R, Spigel DR, et al. High incidence of cetuximab-related infusion reactions in Tennessee and North Carolina and the association with atopic history. J Clin Oncol. 2007; 25: 3644-3648.
- Commins SP, Satinover SM, Hosen J, et al. Delayed anaphylaxis, angioedema, or urticaria after consumption of red meat in patients with IgE antibodies specific for galactose-alpha-1,3-galactose. J Allergy Clin Immunol. 2009; 123: 426-433.
- Centers for Disease Control and Prevention. Alpha-gal Syndrome. Last reviewed July 28, 2023. Accessed September 8, 2023. https://www.cdc.gov/ticks/alpha-gal/.
- Sharma SR, Karim S. Tick saliva and the alpha-gal syndrome: finding a needle in a haystack. Front Cell Infect Microbiol. 2021 Jul 20;11:680264..6. Platts-Mills TAE, Li RC, Keshavarz B, Smith AR, Wilson JM. Diagnosis and management of patients with the α-gal syndrome. J Allergy Clin Immunol Pract. 2020 Jan;8(1):15-23.e1.