Part 3: How We Reached the Brick Wall Blocking Physician Advocacy
Preview this animated timeline providing a brief history of healthcare payment in the United States, which was outlined in Part 1 of this series. Part 2 detailed today’s challenges, why they occurred, and ways we can influence improvement in a broken, inefficient system.
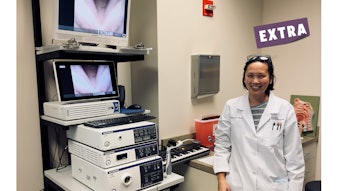
 James C. Denneny III, MD
James C. Denneny III, MD
AAO-HNS/F Executive Vice President and CEO
The current makeup of Congress features small margins for the majority party in both the House of Representatives and the Senate. This has changed the budgetary discussions in the 118th Congress considerably with emphasis on the size of the deficit, national debt, and sustainability of Medicare and Social Security during the inflationary times we are witnessing. It seems unlikely that there will be any significant infusion of new money for healthcare, and it would not be surprising to see a focus on cost control in several areas including the pharmaceutical industry.
How does the current combination of events play out for physicians? The United States already has the most expensive healthcare system in the world, and U.S. physicians have the highest average incomes when compared to physicians in the rest of the industrialized world. The fact that physicians’ income has risen over the past 10 years—despite the unrelenting rise of office overhead from 30%-40% to more than 60% over the last 15 years—is remarkable considering that Medicare reimbursement per Relative Value Unit (RVU) is less than it was in 1998.
Why did the overhead rise so steeply during a period when practice efficiencies were introduced through professional administration? Could it have been unfunded mandates such as electronic health records (EHRs), the Physician Quality Reporting System (PQRS) and MIPS quality programs, complex documentation paradigms, and expanding pre-authorization programs? All of these complex programs necessitated additional equipment and the personnel needed to comply and participate.
There is no mystery that the combination of unfunded mandates caused significant obstruction to efficient practice and required additional hours to the already overburdened physician workload. Furthermore, rapid social change, industry consolidation, the employed status of the majority of physicians, and increasing adversarial relationships with private payers, taken together have created unavoidable burdens on physicians. Throw in COVID-19, and you’ve got the “perfect storm” resulting in the highest level of burnout to date. Almost 70% of otolaryngologists have identified themselves as having significant burnout. In the 2022 Academy-sponsored Workforce and Socioeconomic Survey, 38% of 1,800+ respondents said they would retire tomorrow if they could. (The findings from this 2022 survey will be reported on later this year.)
Otolaryngology, as well as organized medicine, finds itself in a difficult position in regard to legislative, regulatory, and private payer advocacy. At the federal level it is all about the money. With insolvency hanging over the head of the Centers for Medicare & Medicaid Services (CMS), the agency is increasingly reducing Relative Value Scale Update Committee (RUC) recommended values implemented through the annual Medicare Physician Fee Schedule. At the same time, CMS and private insurers are pushing enrollees into Medicare Advantage managed care plans, even though they cost more and have been found to be denying medically necessary care, according to a recent audit conducted by the U.S. Office of the Inspector General.
Federal regulations have turned bipartisan legislation designed to protect patients from excessive “surprise bills” into a tool that healthcare insurance companies employ to make it extremely difficult for physicians to get appropriate payment for their services. If the recent Federal Trade Commission regulation on restrictive covenants is not struck down by the judicial system, this seismic shift will certainly change the dynamics of consolidation of the healthcare system and private equity transitions. There is solid evidence to show that both of these do not lower the cost of healthcare, but instead significantly increase it.
The healthcare insurance industry has been emboldened by the recent regulatory changes as well as the failure to be held accountable for the Medicare Advantage issues. The reality of the matter is that for all intents and purposes this industry acts unilaterally and answers to no one. Since the “No Surprises Act” (NSA) regulations came out, we have had significant problems getting anything but form letters back from commercial insurers in response to legitimate concerns about policy changes that negatively affect patient care. This is a distinctly different relationship from what we previously enjoyed, particularly from United Healthcare, which no longer invites or accepts opportunities to improve policies based on the most current data and clinical practice.
How can we change the narrative to have meaningful input into what is best care? Equally as important, how can physicians deliver this care most efficiently and cost-effectively to the entire spectrum of patients in the U.S. under the current system?
In my opinion this will require a change in the prioritization of our goals for otolaryngologists as well as the rest of the medical community. We need to move away from reimbursement and budgeting as the primary goal and concentrate on what will make circumstances better for practicing physicians. The Academy has been progressively adjusting priorities in our discussions with legislative and regulatory leaders to emphasize the importance of establishing a system that allows physicians and the rest of the healthcare delivery team to spend their time delivering care, not wasting it on administrative duties that have shown no value in improving the overall success of the healthcare delivery system. This does not mean that we have abandoned seeking fair reimbursement for those providing patient care. This approach is consistent with physician surveys that identify the major etiologies of burnout. Most of the top causes are related to frustrations in the delivery of care, whether it be the decline in control of practice, the EMR, barriers to providing care such as pre-authorization, or the multitude of other time and energy sapping administrative duties that add hours to each day. In the 2022 Workforce and Socioeconomic Survey referenced previously in this column, salary (money) played a relatively minor role in dissatisfaction for the majority of respondents.
My hope is that we will be able to interest the various coalitions and alliances we participate in today to adopt similar strategies, so we can work as a more powerful team to help craft a different delivery system. Following are goals we can all get behind, which I believe have a reasonable expectation of success.
- Concentrate on eliminating/minimizing administrative duties that don’t improve patient care yet waste significant amount of resources including time.
- Continue to prioritize outcomes research that cannot be ignored by the insurance industry.
- Advocate for a regulatory approval process at the Food and Drug Administration (FDA) that collects the data necessary to obtain both FDA approval while demonstrating clinical efficacy. This may prevent the blanket application of an “experimental or investigational” label on “new technology” by private insurers.
- Mandate the immediate interoperability of medically related data sources across EMR vendors and hospital systems. The true value of obtaining this data will never be recognized without this intervention.
- Approach patient interest groups as well as employer consortiums and involve them directly to ensure that they receive the benefits they’ve been promised for themselves and their employees by healthcare insurers. These may be the only groups capable of holding the healthcare insurance industry accountable for their actions.
There is evidence that these strategies can be successful. The CMS adjustment to E/M documentation requirements has eased some of the burden that was consuming such a large proportion of physicians’ time every day. The recent CMS proposed rule on pre-authorization followed considerable efforts across the house of medicine for a regulatory response to alleviate the negative effects of prior authorization policies on efficient delivery of care. There is also federal legislation that passed the House of Representatives in the 117th Congress but stalled in the Senate that seeks to accomplish similar goals. The Academy is once again advocating for enactment of this bill in the current Congress.
If we can achieve these goals, we will improve patient care, reduce major stressors that are responsible for physician burnout, reduce the resource and time costs to provide care, and hopefully bring back the JOY in practicing medicine. This pathway can also be successful without adding large amounts of additional funding to the healthcare system, which should make it attractive to governmental decision makers in Congress and federal agencies. The sheer size of the healthcare industry ensures that this change will not happen overnight but will require persistence and patience. However, we should not be satisfied with persistent delays in implementing changes beneficial to all involved. This emphasis on alternative ways to get our messages heard and acted upon does not mean that we will abandon the more traditional methods—the new programs will be additive to our portfolio. Rest assured that your Academy will continue its daily advocacy on your behalf.
Reference
- U.S. Bureau of Labor Statistics. (n.d.). Over 16 million women worked in health care and social assistance in 2021. U.S. Bureau of Labor Statistics. Retrieved March 8, 2023, from https://www.bls.gov/opub/ted/2022/over-16-million-women-worked-in-health-care-and-social-assistance-in-2021.htm