World Voice Day 2023: Q&A
Materials to provide your patients timely advice on taking care of their voices for World Voice Day!
New in 2023! In recognition of World Voice Day, the Voice Committee developed a patient-focused Q&A video, answering common questions about seeing an otolaryngologist/laryngologist for voice symptoms as well as vocal care, conditions, and treatments.
AAO-HNS Voice Committee Members, Thomas L. Carroll, MD, Mark R. Gilbert, MD, Lyndsay L. Madden, DO, and Libby J. Smith, DO, offer additional answers to these questions you may hear in clinic:
Q: What are benign vocal fold lesions and how are they treated?
 Thomas L. Carroll, MD
Thomas L. Carroll, MD
Benign vocal fold lesions (BVFLs) are focal changes to the vibratory layer (lamina propria) of the vocal fold, or the vocal cord, that result in limitations of normal vibration and lead to symptoms including hoarseness, throat clearing, decreased vocal range (can’t hit the high notes), vocal effort, and vocal fatigue. Depending on the size and depth of the BVFL, the symptoms can vary from mild and inconvenient to severe and debilitating. The most common names given to BVFLs are nodules, polyps, and cysts. In addition, fibrous mass and pseudocyst are terms more commonly used by voice-specific clinicians.1
Many otolaryngologists describe how BVLFs evolve from a common injurious event or behavior, while others also believe they can form from normal voice use when talking on top of existing inflammation and swelling from a viral laryngitis, chronic allergies, or reflux that effects the throat.2 No matter how or why they start, BVFLs may be predestined to become a polyp or cyst from the beginning or are theorized to be diagnosed at any point along a spectrum of an evolving lesion (i.e., from nodule to polyp to cyst).3 The vast majority of people who present with BVFLs do not report one event where their voice changed, rather a worsening of symptoms over time that has led them to seek care.
Whether they share a common origin after an injurious vocal event or from normal use in the setting of existing inflammation, BVFLs can have non-distinct appearances on laryngoscopy with stroboscopy (the technological tool used to see vibration of the vocal folds in the outpatient, office setting). For this reason, many laryngologists do not give BVFLs specific names until they either resolve without surgery (nodules or nonspecific vocal fold lesions) or with surgery where either microscopic appearance or pathology report can fine tune the diagnosis to one of the three most common results: fibrous mass/scarring, polyp, or cyst. With high definition videostroboscopy in the office and what can be appreciated under the microscope, it is less common for a laryngologist to call lesions “nodules;” rather, laryngologists give a diagnosis of a clearer, dominant unilateral BVFL and an opposing, reactive lesion (akin to a callous forming from the trauma of the primary BFVL hitting it). The term “nodules,” considered by most to be symmetric and plural by definition, remains widely accepted. This is often a reflection of the technology available as many otolaryngologists do not routinely use high-definition flexible laryngoscopes and videostroboscopy in the office setting.
Treatment of BVFLs usually involves voice therapy with a speech-language pathologist at some stage of care. A surgical intervention to remove the offending BVFL is performed when necessary. The order of therapy versus surgical treatment administered first depends on the patient and pathology. Some patients will do well with voice therapy alone (typically small- to medium-sized lesions), while others with larger BVFLs may require excision before therapy can be completed successfully. Voice therapists who work independently of a laryngologist and are sent a patient with a BVFL that proves not to be amenable to improvement with therapy will often offer education about what to expect from the treatment process to the patient; the therapist hopefully can feel empowered to advocate for earlier procedural or surgical intervention on the patient’s behalf with an intended plan to resume therapy postoperatively. Upfront voice therapy is always worth a try if both the patient is motivated and the therapist sees the potential for improvement at the onset; if one of these two ingredients is missing, the otolaryngologist may need to intervene or refer for surgical care sooner rather than later.
Surgical management of BVFLs is not without risk but is offered when the patient has pursued all other options. Traditionally, BVFLs are removed in the operating room using microlaryngeal techniques under suspension laryngoscopy. A small incision is made next to the lesion, the lesion is dissected from the surrounding normal structures, the lesion is removed, and the overlying normal tissue is replaced. Achieving all these steps is the goal, but this is not always possible. With unintentional, but often unavoidable, loss of normal tissue and the resultant scarring that must occur as the vocal fold heals, the surgeon and patient must be ready for issues with healing postoperatively. Although the routine outcome is often favorable and as expected, the risk of scar formation is often a superior trade-off to what the patient was experiencing from the BVFL preoperatively; but postoperative voice therapy and steroid injections into the forming scar can often mediate these postoperative healing issues to some degree. Newer techniques employing lasers in the office to ablate or soften certain BVFLs are becoming more common, especially for lesions with a vascular or inflammatory component (i.e., hemorrhagic polyps, newer scar/fibrous masses).4
References
- Naunheim M, Carroll T. Benign vocal fold lesions: update on nomenclature, cause, diagnosis, and treatment. Curr Opin Otolaryngol Head Neck Surg. 2017;25 (6):453-458. doi: 10.1097/MOO.0000000000000408
- Lechien JR, Saussez S, Nacci A, et al. Association between laryngopharyngeal reflux and benign vocal folds lesions: a systematic review. Laryngoscope. 2019;129(9):E329-E341. doi:10.1002/lary.27932
- Johns M. Update on the etiology, diagnosis, and treatment of vocal fold nodules, polyps, and cysts. Curr Opin Otolaryngol Head Neck. 2003;11(6):456-461. Cited in: Journals@Ovid Full Text. Accessed February 01, 2023. https://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=ovftf&NEWS=N&AN=00020840-200312000-00009
- Shoffel‐Havakuk H, Sadoughi B, Sulica L, Johns MM. In-office procedures for the treatment of benign vocal fold lesions in the awake patient: A contemporary review. Laryngoscope. 2019;129(9):2131-2138. doi:10.1002/lary.27731
Q: I was told I have glottal incompetence and that is why my voice is bad and why I run out of air when I talk. What does this mean?
 Mark R. Gilbert, MD
Mark R. Gilbert, MD
Glottal incompetence can sometimes be caused by various vocal fold lesions or scars, but usually it is caused by a vocal fold immobility such as paralysis or by severe thinning of the vocal folds called vocal fold atrophy. Treatments for these usually involve augmentation of the vocal folds to restore volume or, in the case of a unilateral paralysis, repositioning of the vocal fold so that the opposite vocal fold can contact it successfully and efficiently. There are options for injection of fillers for correction of glottal incompetence using a variety of substances that, depending on the scenario, can either be performed in the office or in the operating room; these may last from several weeks to a couple of years, or, in the case of a patient’s own fat tissue, may be permanent. However, permanent correction of glottal incompetence most commonly involves a procedure called Type I laryngoplasty (or thyroplasty), with the placement of an implant material into the larynx via open surgery.
Surgical treatment of the glottal insufficiency of vocal fold paralysis more often is able to restore the normal voice than the treatment of vocal fold atrophy, as the latter often is associated with many other changes of the aging voice, which are harder to reverse. In either scenario, voice therapy is often necessary to achieve the best voice outcome, either as primary therapy or as an adjunct to surgery.
Q: Is a sore throat ever normal? When should I seek treatment, and what can I do at home to help?
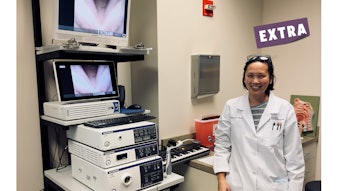
 Lyndsay L. Madden, DO
Lyndsay L. Madden, DO
Sore throats can be caused by several things, including:
- Viruses
- Bacterial infections
- Allergies
- Irritation
- Lesions of the larynx or upper airway
- Voice overuse/misuse
Viral and bacterial infections: Sore throats accompanied by upper respiratory tract infection-like symptoms may be caused by either viral or bacterial infections. Common cold viruses, the flu virus, croup, or mononucleosis are often present in patients with sore throats accompanied by fatigue, fevers, and headache and are usually self-limiting illnesses that are treated with over-the-counter therapies. Strep throat is a common bacterial infection that can cause sore throat related to tonsillitis, pneumonia, sinusitis, scarlet fever, and/or ear infection. Pertussis, or whooping cough, can also cause sore throat with a classic “barking” cough that can cause sore throat and severe symptoms, especially in unvaccinated and young individuals. The most common dangerous throat infection that otolaryngologists see is called epiglottitis. This causes severe and often rapid swelling of the airway, which requires emergency medical intervention. Epiglottitis is diagnosed by imaging studies and/or laryngoscopy. Bacterial infections are treated with antibiotics.
Allergens and irritation: Inhaled allergens can cause inflammation to the lining of the upper respiratory tract, leading to soreness of the throat. Irritation from dry air, pollution, or chemical exposures can lead to inflammation of the upper airway, also leading to throat soreness.
Laryngeal or other lesions of the upper airway: Lesions of the upper aerodigestive tract can be the cause of pain and are often accompanied by otalgia. Patients may also report a hoarse voice. If a patient has throat pain and hoarseness that is persistent for three or more weeks, this warrants a laryngeal scope exam.
Voice overuse/misuse: Individuals who have high vocal demands or unhealthy vocal habits may present with a sore throat accompanied by hoarseness. Voice overuse/misuse may lead to benign vocal fold lesions or functional voice conditions. If a patient is experiencing pain associated with voicing, a laryngeal exam is warranted.
Signs and symptoms of sore throat can widely vary depending on the cause. Signs and symptoms may include pain that is worse with talking or swallowing, difficulty swallowing, swollen or red tonsils, sharp or dull aching pain in the throat, swelling of the neck, hoarse or muffled voicing, cough, fever, body aches, headache, and/or nausea.
Signs and symptoms that warrant medical attention include:
- Difficulty breathing or swallowing
- Unusual drooling
- Sore throat that lasts more than one week
- Difficulty with mouth opening
- Joint pain
- Earache
- Rash
- Fevers higher than 38.3○C
- Bloody saliva or phlegm
- A lump or swelling of the neck
- Persistent hoarseness for more than three weeks
- Facial swelling
Aside from medical therapies that may be required for treatment of the aforementioned conditions, there are several lifestyle modifications that may be trialed for soreness of the throat.
- Rest: Resting the body and voice may be beneficial.
- Avoid irritants: Known irritants such as smoke or cleaning products should be avoided.
- Humidification: Using a cool-air humidifier to eliminate dry air that may further irritate a sore throat can be beneficial.
- Drinking fluids: Fluid consumption may be helpful in preventing dehydration, which leads to laryngeal dryness and further irritation.
- Lozenges: Lozenges may provide comfort to a sore throat. It is important to avoid menthol-containing agents.
- Comforting food and beverages: Warm liquids such as decaffeinated teas, broths, and warm water with lemon and honey can be quite soothing to a sore throat, as can cool treats such as popsicles.
A free informational video from ENThealth covers the topic of sore throats by Lisa Perry-Gilkes, MD. ENThealth also offers wellness and prevention information with Seven Tips to Help You Prevent a Sore Throat.
Q: I’m smoking a “natural” substance, so how bad could it be to my voice?
 Libby J. Smith, DO
Libby J. Smith, DO
In the past decade, vaping became the new thing. This is now being compounded by increased cannabis use with legalization in many states for medical and recreational use. Although physicians are conditioned to ask patients about tobacco smoking and chew, we now need to add vaping and marijuana use to our social history questions.
Smoking any substance must pass through the vocal folds on its journey to the lungs. The heat and chemicals can be injurious to the sensitive mucosal lining of the vocal folds. In the case of tobacco smoking, this can result in dysplasia/cancer, which requires definitive treatment. It can also result in proliferation of the superficial lamina propria, which is called Reinke’s edema, polypoid corditis, polypoid degeneration, among other names. Patients, usually women, present to clinic with complaints of low vocal pitch, being mistaken for a man (especially on the phone), and in extreme cases even dyspnea. Surgery is often employed to help with voice quality and to decompress the lesions to improve the glottic airway. Debate has existed on the necessity of smoking cessation prior to phonosurgery (surgery to improve voice), but when dyspnea is present, surgery is indicated.
With legalization for medicinal reasons, particularly for chronic pain, nausea, and poor appetite, cannabis use is increasing. Recreational use is also legal in several states. As the legal and social acceptance of cannabis use changes, it is possible that its use in all venues will continue to increase. In 2019, a study of self-described smokers found that in-home cannabis smoking is more prevalent than in-home tobacco smoking.1 Despite the possible positive aspects of cannabis use, there are potential negative side effects. Unfortunately, it can affect memory (short-term especially), slow executive processing, and reduce attention. Chronic marijuana use and use at an earlier age are risk factors for neurocognitive deficits with reduced brain volume and density.2 These effects are important to know and understand so we can better counsel and treat our patients.
Cannabis can be ingested by smoking, vaping, or eating edibles. From a laryngologist’s perspective, this is intriguing since there are anecdotal suggestions that taking cannabis in a nonsmoking form results in less vocal impact, which makes sense when we learn about the physical sequelae of different modes of cannabis consumption. Smoking has historically been the common mode of consumption, generating temperatures up to 600°C-900°C as well as toxic byproducts. Vaping is becoming more popular as a smokeless form. Generated temperature is less, 160°C-230°C, with fewer caustic byproducts. Edibles and oil extract mitigate both the negative aspects of heat and toxic byproducts; however, dosing may be more variable,3 resulting in higher risk of overdose.
In 2022 an anonymous survey study of adult voice patients reported their marijuana use in terms of frequency, modes of consumption, and associated self-perceived voice changes. In this cohort, smoking and vaping were equally prevalent. Self-reported voice changes occurred least often with edibles, followed by vaping, with smoking garnering the most associated self-reported voice changes.4 We do not yet know if chronic smoking of cannabis results in the same effects as chronic tobacco smoking. We do not yet know if or how much vaping is “better” for the larynx long term. Future research is needed to answer these questions.
In honor of World Voice Day, please inquire about smoking and vaping (any substance) to your battery of social history questions. As we meet patients where they are, we can counsel them on modes of consumption and mitigating risk to the vocal folds. In so doing, we are better able to provide counsel to and advocate for our patients and their vocal folds!
References
- Bellettiere J, Liles S, Posis AIB, et al. In-home cannabis smoking more prevalent than in-home tobacco smoking among 2019 Global Drug Survey respondents. Addict Behav. 2022 Feb;125:107130.
- Urits I, Charipova K, Gress K, et al. Adverse effects of recreational and medical cannabis. Psychopharmacol Bull. 2021 Jan12;41(1):94-109.
- MacCallum CA, Russo EB. Practical considerations in medical cannabis administration and dosing. Eur J Intern Med. 2018;49:12-19.
- Balouch B, Alnouri G, Valentino W, Sataloff RT. The effect of marijuana on the voice: a pilot study. J Voice. 2022;36:559-562.