What Should the Comprehensive Otolaryngologist Know about Voice Care?
Three laryngologists with the Bastian Voice Institute discuss vocal over-doer syndrome, fiberoptic laryngoscopy versus videostroboscopy, muscle tension dysphonia management, and more.
Interviewer:
Jordan I. Teitelbaum, DO, Voice Committee member
Interviewees (all laryngologists):
Rebecca C. Hoesli, MD
Robert W. Bastian, MD
Brent E. Richardson, MD
Note: The following interview has been edited for clarity.
 The Bastian Voice Institute is a private practice subspecialty laryngology group in the Chicagoland area that treats all aspects of voice, swallowing, and airway disorders.
The Bastian Voice Institute is a private practice subspecialty laryngology group in the Chicagoland area that treats all aspects of voice, swallowing, and airway disorders.
Q: I see a lot of non-singer/actor professional voice users—people who have to use their voices a lot at work, like teachers, fitness instructors, coaches, salespeople, healthcare workers. What advice should we give?
Dr. Hoesli: We talk with them about vocal over-doer syndrome. They can be overusing their voice, and over time, that can result in classic nodules, polyps. We talk about the usage of the voice and the amount, the manner, and the spacing. Those are the three main things that lead to vibrational trauma. We talk about monitoring and modulating those three things.
Dr. Bastian: We show instructional videos and teach self-monitoring to amplify their own awareness of vocal cord swelling.
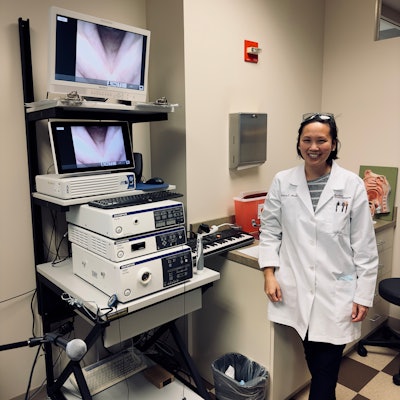 Dr. Rebecca Hoesli, MD, a fellowship-trained laryngologist, in her videostroboscopy room. It's not every day you see a doctor's office equipped with a microphone and electric keyboard.
Dr. Rebecca Hoesli, MD, a fellowship-trained laryngologist, in her videostroboscopy room. It's not every day you see a doctor's office equipped with a microphone and electric keyboard.
Dr. Hoesli: With Zoom, it’s kind of interesting. I’m seeing either overusage or underusage. Same thing with masks. We recommend using headsets and microphones so that patients can talk at a normal level. For overusers, definitely hydration is the primary thing. That allows the vocal cords to be lubricated. It’s also important to reduce inflammation as much as possible.
Dr. Bastian: We teach everybody to do vocal cord swelling checks, and it gives people a way to monitor their own vocal cords using very high-pitch, low-intensity voicing. Other important things are self-monitoring and prevention.
Dr. Richardson: Patients should try to figure out what are the parameters of their voice issues—when they have been talking a lot, when they haven't been talking at all. What part of their voice is the problem? What does hoarseness mean to them? We have to make sure we're talking about the same thing.
Q: I might be the only rhinologist on the Voice Committee of the American Academy of Otolaryngology–Head and Neck Surgery. Does postnasal drip (PND)/sinus drainage affect the voice? What nasal sprays do you like prescribing?
Dr. Hoesli: When I talk to people about voice, it’s primarily about how they use the voice. Any type of inflammation on top of that can contribute. PND, allergies, coughing—they count as voice usage. If patients have symptoms of allergies or acid reflux or rhinitis, we have them do trials of therapies. We love those nasal saline mists and saline rinses.
Q: What are we missing on flexible and fiberoptic laryngoscopy that you see on videostroboscopy?
Dr. Hoesli: The strobes are best for showing the flaccidity of the vocal cords. You can also differentiate between actual types of vocal fold trauma.
Q: You work closely with speech-language pathologists and voice therapists. What should I tell patients when they ask me why I’m recommending speech therapy?
Dr. Hoesli: Speech therapists are the best ones to help implement the exercises that need to be done inside the throat. I tell people that when they have bad posture of the back, it's relatively easy for us to fix that manually to move you where I want you to be. Inside your throat we can't do that. It's really hard to do that when you can't see. So the speech therapists are really helpful for giving patients exercises to simulate what they want them to do, as if they're putting them in that good position.
Q: What is the latest with muscle tension dysphonia management?
Dr. Hoesli: Muscle tension dysphonia, as we define it here, is very specifically the compensatory contraction of the pharynx and incomplete closure between the glottis. There's a space between the vocal processes, and you'll see that contraction of the pharynx that patients use to help them make their voice. You'll see that start to elevate. Really, it's working with the speech therapist to eliminate this.
Q: I have seen so much sensory neuropathic cough (SNC) recently. I wish I knew more about it. Where should I start, and what would empiric therapy be?
Dr. Bastian: It's a syndromic diagnosis. SNC is particularly syndromic. In about a third of people there are subtle movement abnormalities in the cords, but in most people there are no findings. It is prima facie; it is not a diagnosis of exclusion. Patients have been treated for the usual suspects: allergy, acid reflux, and asthma. If you want to hit the nail on the head, it’s very labor intensive. We have eight different treatments, and there is a lot of follow-up, phone calls, portal messages.
We start patients with 10 mg of amitryptaline two hours before bed and then they up-titrate according to response. It's rare that people need more than 50 mg. I use desipramine or nortryptyline in patients over 65. For lots of people, you don't ever get them beyond 80% reduction.
Q: What’s the latest and greatest in laryngopharyngeal reflux?
Dr. Hoesli: I really like Gaviscon Advanced (liquid) if patients have signs of inflammation of the vocal cords—redness, swelling of the interarytenoid space.
Dr. Bastian: Fair enough if reflux therapy makes them better, but if not, it's time to find a new diagnosis.
Dr. Richardson: The symptoms are the thing that leads the treatment. If they truly have symptoms that are attributable, and you do a therapy trial. Everyone has some degree of reflux. The question is does it cause problems.
Q: What conditions do you wish got sent to you more often, more promptly, or in the first place?
Dr. Bastian: Any patient who complains of voice change, but there's nothing seen to explain it. Otherwise, people get a delayed diagnosis. If the person is steadfast in saying, “There is something wrong with my voice,” they need to be seen.
Dr. Hoesli: They tried reflux meds, they tried allergy meds, and they still have voice change. Or, it got bad and is not getting better in three weeks, or it got bad and is getting progressively worse.
Dr. Bastian: The people I'd like to see sooner are those who say, “Something is wrong,” and they don’t get an answer; there is no clear explanation. When they persistently say something isn't right, but they’re told everything looks fine.