Part 2: How We Reached the Brick Wall Blocking Physician Advocacy
Part 2 of this series details today’s challenges, why they occurred, and ways we can influence improvement in a broken, inefficient system.
James C. Denneny III, MD, AAO-HNS/F Executive Vice President and CEO
 James C. Denneny III, MD
James C. Denneny III, MD
AAO-HNS/F Executive Vice President and CEO
I intentionally left out the incendiary event that triggered a perfect storm consisting of the explosion of federal spending through legislation, aggressive regulatory policies, previously unimaginable scope-of-practice expansion, and the unprecedented power now wielded by the insurance industry, all in the name of patient access. COVID-19 accelerated the march toward the fulfillment of two personal predictions I made almost a decade ago that we are now currently witnessing: First, “scope of practice will continue to expand until morbidity and mortality rein it in,” and second, “Medicare Part B will not be fixed until patient access declines.”
Like Sir Winston Churchill said in the mid-1940s as the world approached the end of WW ll, “Never let a good crisis go to waste.”
All of the major pieces of this puzzle are on now on the table. Let’s examine how they fit together, including the how and the why they are contributing to current positions. The federal government recognized early on that the initial projections for Medicare Part B spending, which initially allowed the government to give a significant benefit for minimal expense, would change dramatically if life expectancy or the population increased, particularly for men.
Federal officials also realized they faced the same scenario with the Social Society Administration. The average length of life increased from 66 to 80 years old, a roughly 20% increase. The first cost control program put in place for Medicare and de facto for private insurers was the creation of the resource-based relative value scale (RBRVS) system of a resource-based payment for medical services. Rather than get involved “in the trenches” warfare that would decide the value of each service, the Centers for Medicare & Medicaid Services (CMS) wisely employed the American Medical Association (AMA) to do this. This created a source of revenue for the AMA that they cannot do without and helped ensure a cooperative and symbiotic relationship that would later be used to affect policy change.
Realizing the rapid growth of the healthcare delivery complex, CMS added the Sustainable Growth Rate (SGR) in 1997, which along with its successor Medicare Access and CHIP Reauthorization Act (MARCA), have forced physicians into an annual fight for a “break-even” position for Medicare reimbursement and added significant requirements to get there. Despite these steps, including managed care and value-based care, the exorbitant increase in administrative costs for the system and the resultant significant shift in the physician cost of services, the overall cost for healthcare services in the United States continues to increase. The per capita cost for healthcare in the U.S. dwarfs that spent by other countries, and we still achieve the lowest grades of the 11 major industrialized countries for our overall healthcare system. Without question, the COVID-19 pandemic exposed the access issues and inequities built into the current system.
Quick question. Who were the biggest winners, not including politicians, of the COVID-19 pandemic? The health insurance industry reported record profits during the pandemic, including the third quarter 2022 record earnings below:
- UnitedHealth Group: $5.3 billion, up over 28%
- Cigna: $2.8 billion, up over 70%
- Elevance Health: $1.6 billion, up over 7%
- Humana: $1.2 billion, down 20%
- Centene: $738 million, up over 26%
- Molina: $230 million, up over 60%
Profits rose each year of the pandemic as follows: Profits in 2021 rose to $17.3 billion, up from $15.4 billion in 2020 and $13.9 billion in 2019. Much of this was related to care that was not given because of public concern and lack of availability for elective care. These record profits have not prevented the industry from “crying poor” and launching widespread assaults on physician reimbursement through policies that are essentially not overseen by anyone.
That leaves us with the non-sequitur knowledge that the healthcare delivery complex spends the most and delivers the least quality. The results have not changed despite spending an unprecedented percentage of gross domestic product (GDP) on healthcare delivery. The overall pie has continued to grow, despite shifting percentages for each provider group. The U.S. system spends three times what any other healthcare system does on administration, which was supposed to rein in costs but has only added an additional cost burden.
Politically each attempt to significantly change the healthcare system has resulted in the political party trying to make the change being voted out of office (not a singular issue). This fact alone has been a significant deterrent to real healthcare reform. The list of administrations that have attempted reform includes those of Presidents Harry S. Truman, Lyndon B. Johnson, William J. Clinton, and Barack H. Obama.
Given the difficulty of major legislative activity over the last six years, the government has turned to regulatory policies to put the clamps on spending in both the governmental funded and private insurance market. These policies have resulted in the unprecedented boldness by many groups seeking expansion of scope of practice at the state level as well as that of the private healthcare insurance industry.
During the pandemic and Public Health Emergency (PHE) under the broad umbrella of “expanded access,” there were significant changes to the telehealth programs and a loosening of the supervision rules of payment for residents as well as advanced practice providers (APPs). Some of the changes have been made permanent, and there is now extensive activity in state legislatures across the country seeking to expand the scope of practice of several key groups that work with otolaryngologists. Most notably, the physician assistants (PAs), who want to eliminate the requirement for supervision despite the fact their training is based upon the principle of physician supervision, and the audiologists, who have sought to expand their scope through multistate licensing and just recently, in Maryland, seeking the equivalence of physician status through MD House Bill 401. This bill states that those who “Practice audiology” would allow audiologists to “order, evaluate, diagnose, manage, or treat any auditory or vestibular condition in the human ear.” Sounds like the same wording as state licensing and hospital privileging for physicians, doesn’t it?
Physicians spent a lot of time and resources advocating for relief and protection for patients who were victimized by exorbitant unexpected medical bills that were impossible for many to pay. Working with bipartisan supporters in Congress, a compromise bill, the “No Surprises Act (NSA)” was passed and signed into law by President Joe R. Biden. As the saying goes, “the devil is in the details,” and how true that turned out to be when the administration released the proposed regulations and rules for this new law. Physicians and hospitals had been stabbed in the back by regulations that required additional roadblocks and costs to practice medicine. These rules might as well have been written by the insurance industry itself. The Qualifying Payment Amount (QPA) and the Independent Dispute Resolution (IDR) tilted the playing field so far that they have been struck down by federal judges in four rounds of lawsuits to date. However, the damage has been done and many aspects are currently in place as a final resolution has not been achieved in the courts. It is all about the money, not fairness.
The insurance industry has always carefully protected its margins and justifiably monitored clinical indicators and data as guidance for coverage decisions. For many years, there was a collegial working relationship between most of the insurance companies and organized medicine with reasonable discussions occurring frequently. Both sides had a shared interest in preventing inappropriate and abusive utilization practices that put patients at risk and wasted resources that could be better allocated elsewhere.
COVID-19 and the NSA have changed all of that. The symbiotic relationship between the insurance industry and the federal government that has existed for decades under the surface is now out in the open. These recent regulatory actions have clearly identified the insurance industry as an important tool separate from the government for policy change as directed. The current situation with the government relying on the industry so heavily has resulted in no effective oversight and emboldened actions that I have not seen before.
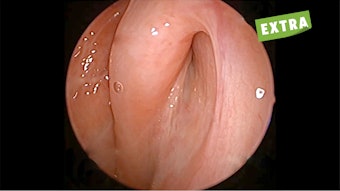
Was it a coincidence that the biggest of them all, United Healthcare (UHC), announced a policy in December 2021 that resulted in a non-negotiable coverage policy change that eliminated over 200 new technology procedures across a broad array of specialties? They were not willing to review evidence or discuss this policy change with specialty societies. Surprise! Surprise!
UHC stated that if patients wanted these procedures they would be classified as “private pay.” This would automatically insert them into the NSA mandated IDR if they “chose” to have any of these procedures performed. Somehow, the patients who might benefit from these services but couldn’t afford them without insurance were forgotten. Most recently, UHC has unilaterally decided that home immunotherapy for systemic allergies was investigational and would no longer be covered. This is despite continued coverage for in-office immunotherapy, which is exactly the same preparation used at home. They refuse to even discuss this October 1, 2021, policy change with the American Academy of Otolaryngic Allergy (AAOA) and American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS), despite repeated and multiple attempts. Who is the big loser in this one? The patient!
CMS and Congress agreed with MedPAC’s assessment and recommendation years ago that Medicare Advantage (MA) Plans were a vehicle to save money for the Medicare program. Unfortunately, this projection was no more accurate than many of their other predictions. There is a reason that so many insurers promote Medicare Advantage so heavily: Massive profits. The biggest of these is UHC. Ongoing litigation over auditing and overpayment to MA plans has dragged on for more than a decade with billions of dollars of overpayment at issue. On top of that, a recent investigation by the Office of Inspector General (OIG) found that the plans were denying care through pre-authorization denials at 13% higher than justified by chart review and an additional 18% of payment denials that were not justified. If an individual physician or practice was found guilty in a court of law of the same violations, they would be in jail. What was the consequence for the Medicare Advantage insurers? Nothing! These Medicare Advantage plans are targeted to include 50% of beneficiaries by the year 2030, and at the current rate of yearly cost increases compared to traditional Medicare (4.4% versus 5.3%), it will cost Medicare an extra $182 billion by 2030.
There has also been considerable justifiable concern about the significant increase in billing for healthcare services due to consolidation of hospital systems, physician practices, and ambulatory surgery centers (ASC). This includes private equity buyouts of physician practices and ASCs as well as insurers buying practices in outpatient centers. Instead of a typical business model that features cost savings, the same model in the healthcare industry significantly increases costs all around as each entity strives to maximize profits. The power of the combined lobbyists of these groups makes legislative action all but impossible.
Enter the Federal Trade Commission (FTC) and their sudden interest in employee contracting. There have been debates for decades about restrictive covenants and non-compete agreements as part of employment contracts at the state level where laws and enforcement vary significantly. On January 5, 2023, the FTC announced a proposal to end the use of non-compete clauses in employee contracting. The comment period ends April 19, and if the final rule maintains the language of the proposed rule, it will most certainly be challenged in court. If this regulation survives court scrutiny, how can it affect healthcare contracting? Clearly, it will change the dynamics of private equity buyouts, hospital purchases of physician practices, and employment contracts of physicians and other employees within practices, as well as myriad other healthcare-related contracts. This has the potential to put a damper on these transactions and theoretically at least slow down the escalation of costs generated by these entities and save the system money.
So that leaves otolaryngologists as well as the rest of the house of medicine in a difficult situation. At the core, physicians chose to practice medicine to take the best possible care of patients. There seems to be no limit or end to the unfunded obstacles placed before physicians to run an efficient and effective practice while absorbing the continually escalating practice expenses. This applies not only to private practitioners but also to employed physicians even though this expense is not borne directly by them. The ability to advocate for fair treatment from insurance companies is all but gone following recent regulatory changes and the current relationship with the government. And the government itself must be most concerned about additional spending. These entities stacking the bricks to a higher and wider physician advocacy brick wall take advantage of the fact that we put patient care first above all else.
Where do we go from here? Part 3, the final installment in this series, which you will find in the April Bulletin, will delve into options that might change our situation.