Phonotraumatic Vocal Fold Lesions: 10 Steps to Better Phonomicrosurgery
These steps provide suggestions for navigating phonotraumatic lesions.
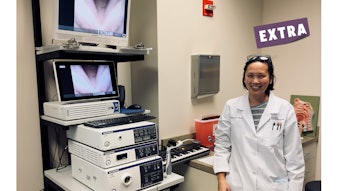
Lesley F. Childs, MD, and Clark A. Rosen, MD
Optimal management of phonotrauma, manifesting as benign mid-vocal fold lesions, centers around a combination of diagnostic and therapeutic nuances. Many patients with these lesion(s) will improve with nonsurgical treatment (such as voice therapy) but some patients will require surgery to optimize recovery of vocal function. At the core of phonomicrosurgical considerations are two fundamental questions: whether to operate and when to operate. Once these tough questions have been answered, a deliberately curated surgical approach optimizes a successful outcome. The following 10 steps provide concrete suggestions for a straightforward approach to navigating phonotraumatic lesions; these are adapted from our course, “Vocal Nodules, Polyps, Cysts: Diagnosis and Current Treatment,” presented at the AAO-HNSF 2022 Annual Meeting & OTO Experience.
Step 1: Accurate Diagnosis
Videostroboscopic laryngeal examination provides important and necessary information surrounding the vibratory parameters and mucosal wave of the vocal folds, allowing for the most accurate diagnosis. Vocal fold nodules, polyps, and cysts have unique and distinguishing features on stroboscopy. Documentation and a patient-centered discussion regarding these features also facilitate specific comparisons before and after intervention, whether nonsurgical or surgical. Videostroboscopy, the “audiogram of the voice,” is an essential component of modern-day voice care.
Step 2: Voice Therapy
Voice therapy achieves improved patient awareness of vocal patterns and helps to rebalance the vocal subsystems, increasing vocal efficiency. Speech language pathologists who specialize in the voice typically partner with an otolaryngologist throughout the patient’s care pathway. Reversibility is possible in most cases of phonotrauma lesions, the extent to which, however, is variable among lesion types and individuals. High-quality voice therapy increases the likelihood of reversibility and sometimes is the only intervention required. Voice therapy optimizes vocal function and thus may result in resolution of voice handicap; sometimes this happens even without the lesion(s) going away completely. This result is acceptable since it is about function not form. Typical duration of voice therapy is four to six sessions. In situations where vocal impairment persists after voice therapy, the skills obtained from behavioral intervention are invaluable in the postsurgical recovery period and beyond. Telehealth voice therapy is now a possibility for many who live in remote regions and for those who otherwise would not be able to attend in-person sessions.
Step 3: Timing of Phonomicrosurgery
Once the decision to operate has been agreed upon, the surgical timing centers around the ability to rest and recover vocal function following surgery. In professional voice users and singers, financial ramifications will undoubtedly affect the timing. With the patient’s permission, inclusion of a performing artist’s manager in the surgical and recovery timing discussions reduces potential conflict. Incorporating voice therapy techniques and training during the vocal ramp-up postoperatively addresses the inevitable vocal deconditioning. It is critical for the surgeon and patient to have a mutual understanding that phonomicrosurgery is not considered a “quick fix” and nothing to rush into. Furthermore, an emphasis on function over form when considering vocal fold surgery underscores the importance of prioritizing voice quality and endurance over subtle stroboscopic abnormalities with no acoustic or functional significance.
Step 4: Informed Consent
Phonomicrosurgical intervention is associated with obvious risks involving both speaking and singing voice quality. During the informed consent process, it is key to outline realistic expectations surrounding the process of voice recovery in the postoperative period. Additional risks include dental or gum injury from the direct laryngoscopy and jaw and neck discomfort. Taste disturbances can temporarily result from the tongue pressure exerted by the laryngoscope. Although taste changes can last several weeks, they nearly always resolve completely. Obtaining permission to potentially address the contralateral vocal fold in the setting of a reactive injury could prevent the need for further phonomicrosurgical procedures if the reactive change does not resolve spontaneously as anticipated.
Step 5: Perioperative Issues
Collaborating with the anesthesia team prior to the start of the case greatly reduces unnecessary risk. If an endotracheal tube is part of the ventilation plan, the smallest possible tube will allow for maximal working room and the least likelihood of vocal fold or laryngeal injury (usually a 5.0 endotracheal tube is used). Additionally, high-flow nasal ventilation can be an effective option for certain patients. The need for strict voice rest postoperatively will also impact the anesthetic wake-up plan. Perioperative steroids, glycopyrrolate, and topical lidocaine are also considerations to discuss with the anesthesia care team.
Step 6: Patient Positioning and Laryngeal Exposure
The ideal patient positioning during phonomicrosurgery allows for the largest laryngoscope, which affords the widest field of view and working room. A sniffing position, with the neck flexed and head extended, provides the most direct access. This positioning is most safely achieved with an articulated headpiece of the operating room table. Familiarity with the various suspension devices aids in the exposure process. Given the dental pressure associated with rigid instrumentation, either a reinforced dental guard or heated dental splint should be used.
Step 7: Telescopes and Magnification
Using telescopes through the suspended laryngoscope provides three-dimensional visualization of the vocal fold free edge and provides a perspective to appreciate the vocal fold’s vertical dimension. Photodocumentation with both a 30-degree and 70-degree telescopic view pre-, mid-, and post-excision is useful for both patient and surgeon. Understanding the relationship between a variable or fixed focal length and the associated magnification of the microscope is critical in achieving maximal magnification, which is essential for precision phonomicrosurgery.
Step 8: Microlaryngeal Instruments
Specialized microlaryngeal instrumentation facilitates precision microsurgery. Familiarity with the delicate instrumentation and care during the sterilization process will help to maintain the integrity of the specific pieces in each set. Attempting to use larger instrumentation is much more likely to cause injury during the excision process.
Step 9: Surgeon Ergonomics
Proper surgeon positioning reduces the likelihood of musculoskeletal symptoms after phonomicrosurgery. A combination of proper arm support and head positioning lends themselves to improved comfort. The concept of bringing the patient to the surgeon once laryngeal exposure has been achieved reduces the surgeon’s muscular fatigue.
Step 10: Microsurgical Pearls
The overarching goal of microsurgery on the vocal folds is to preserve all uninvolved tissue. A bimanual approach with supported arms increases the ease of excision. A submucosal infusion of either saline or diluted epinephrine in certain cases can aid in visualization and hemostasis and could be considered. Allowing plenty of time to avoid rushing and remaining patient during the excision are both fundamental to the best outcome.
Phonomicrosurgery, when executed in a deliberate and methodical fashion, is an elegant means of excision that ideally heals without any evidence of prior intervention. By carefully considering factors, including the timing of intervention, patient and surgeon positioning, as well as the instrumentation and microsurgical techniques employed, successful outcomes are consistently and more easily achieved.