All Flaps Are Not Free: Alternatives for the Reconstructive Surgeon
Although free flaps have completely revolutionized reconstruction of the head and neck, they are not without drawbacks.
T.J. Gal, MD, MPH
First, let me be very clear. I am a microvascular surgeon. I love free flaps. They are the gold standard for reconstruction of most large, complex head and neck defects. There is a large armamentarium of flaps with wide versatility and good functional and aesthetic outcomes. This battle has been won.
So why the discussion of regional flaps?
A regional flap is tissue, primarily soft tissue, with a pedicled axial blood supply that is not adjacent to the defect. There is usually low donor site morbidity that can be closed primarily. Harvest and transfer require much less time, decreasing operative expenses, and potential morbidity. This is in contrast to a free flap, where the tissue and its blood supply are from another part of the body, requiring vascular anastomosis to recipient vessels, usually in the neck.
Historically, however, the primary regional flaps at the disposal of the head and neck surgeon were the deltopectoral and pectoralis major flaps. Although they are “better than nothing,” both flaps had tremendous limitations. The pectoralis flap was often too bulky. Both flaps had limitations in flap size and length that made their versatility somewhat limited. There also was often the need for delayed procedures, debulking, and sectioning—all for a less than optimal result.
Although free flaps have completely revolutionized reconstruction of the head and neck, they are not without drawbacks. There is a significant increase in operative time, even in the most experienced hands. There is the need for microvascular expertise. Flap loss can be catastrophic. Prolonged operative time and takeback procedure can increase patient morbidity. There are increased monitoring requirements, not to mention the increased expense.
Although there are clearly strong arguments on both sides of the free flap/regional flap debate, it is not really an argument. The goal is to find the right flap for the right patient. The utility of the submental island and the supraclavicular artery island flaps has revitalized enthusiasm for the regional flap in head and neck reconstruction. The goal is to provide equivalent reconstruction to a free flap without a free flap. These flaps provide adequate size, pliability, and versatility without the need for microvascular reconstruction. They may also overcome morbidity concerns in patients too sick for free flaps.
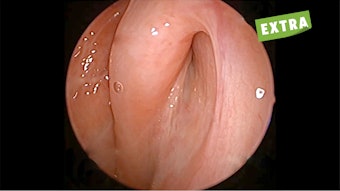
The submental artery flap was first described in 1993.1 It is based off the submental artery and vein, which are branches of the facial vessels. It is harvested at the time of the neck dissection, as the pedicle is dissected off the submandibular gland and is generally harvested in 30 to 60 minutes. The resulting submental defect can be closed primarily with minimal additional elevation of the neck flaps. It is ideal for defects of the floor of mouth and lateral tongue but can also be used for the palate and skin of the face. While it is generally contraindicated in the setting of bulky level I adenopathy, smaller nodes of concern are easily dissected out of the flap pedicle with no effect on oncologic outcome.2 Reconstructive outcomes compare favorably with the radial forearm free flap (Figure 1).
 Figure 1a. Lateral tongue defect reconstructed with a radial forearm free flap.
Figure 1a. Lateral tongue defect reconstructed with a radial forearm free flap.
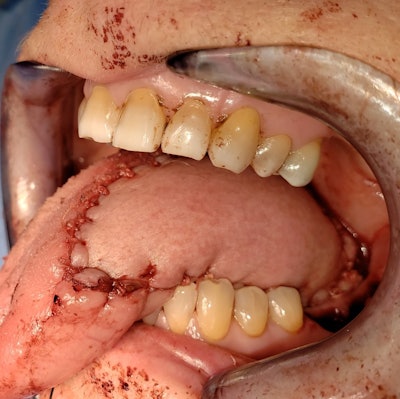 Figure 1b. Comparable defect with a submental island flap.
Figure 1b. Comparable defect with a submental island flap.
The supraclavicular artery island flap has a much longer, complicated history with variations of the flap dating back to Mütter in the mid-19th century.3-5 The supraclavicular artery is a branch of the transverse cervical artery. Venous drainage is through the transverse cervical and external jugular vein. The artery itself is difficult to identify surgically, but presence of an intact transverse cervical artery confirms its presence. In its current iteration, the flap is more anteriorly situated on the deltoid, with a vascular territory extending from the trapezius posteriorly to the deltopectoral groove anteriorly, including the soft tissue of the clavicle. Any unneeded skin can be de-epithelialized to convert an axial flap to an island flap. It is ideally situated for cutaneous defects of the face and lateral temporal bone (Figure 2). It has the advantage of being able to reach above the zygoma, which is challenging with a pectoralis flap. However, it also provides excellent coverage for laryngopharyngeal defects (Figure 3). Flap size can be larger than the submental island flap and can be used for oropharyngeal defects where the submental island flap is not available or insufficient. The flap is harvested in well under an hour. The donor site can be closed primarily, although occasionally a skin graft over the deltoid is needed for larger flaps.
 Figure 2. Facial defect reconstructed with a radial forearm free flap.
Figure 2. Facial defect reconstructed with a radial forearm free flap.
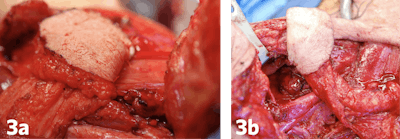 Figure 3a and 3b. Laryngopharyngeal defects closed with the supraclavicular artery island flap.
Figure 3a and 3b. Laryngopharyngeal defects closed with the supraclavicular artery island flap.
The ease of harvest and broad utility of these flaps for soft tissue reconstruction allow for the training of residents in the procedures without the need for microvascular reconstruction. I have trained residents who have gone on to incorporate these flaps into their practices. Reduced monitoring needs and shorter hospital stays make these flaps very “resident friendly.” From the attending side, one concern is that while a soft tissue free flap (CPT 15757) is about 37 relative value units (RVUs), a submental or supraclavicular flap (CPT 15740) is only about 10 RVUs. However, with the significant time saving of the procedure, it is easy to make up or exceed the difference with the ability to add additional cases on to the day, taking care of more patients in the process.
In summary, while free tissue transfer remains the gold standard for soft tissue head and neck reconstruction, the submental artery and supraclavicular artery island flaps provide reasonable, equivalent alternatives to free flaps under appropriate circumstances. The role of these regional flaps should be given strong consideration as a flap option moving forward.
References
- Martin D, Pascal JF, Baudet MD, et al. The submental island flap: a new donor site. anatomy and clinical applications as a free or pedicled flap. Plast Reconstr Surg. 1993;92:867-873.
- Howard BE, Nagel TH, Donald CB, Hinni ML, Hayden RE. Oncologic safety of the submental flap for reconstruction in oral cavity malignancies. Otolaryngol Head Neck Surg. 2014;150(4):558-562.
- Mutter TD. Case of deformity from burns relieved by operation. Am J Med Sci. 1842;4:66.
- Busche MN, Pallua N. Evolution in Flap Design: From the Supraclavicular Artery Island Flap to the Anterior Supraclavicular Artery Perforator Flap. J Reconstr Microsurg. 2016;32:242-244.
- Pallua N, Machens HG, Rennekampff O, Becker M, Berger A. The fasciocutaneous supraclavicular artery island flap for releasing postburn menosternal contractures. Plast Reconstr Surg. 1997;99(7):1878-1884.