HPV-Related OPSCC in APAC Countries
The changing trend in Asia-Pacific countries related to prevalence, diagnosis, and treatment of HPV-related oropharyngeal squamous cell carcinoma is discussed.
Chung-Yu Hao, MD, Sheng-Po Hao, MD, Lim Chwee Ming, MMed, MRCS, and Hidenori Inohara, MD, PhD
The oropharyngeal squamous cell carcinoma (OPSCC) is recently recognized as a distinct cancer based on human papillomavirus (HPV) status. The effect of HPV positivity on immunochemistry is significant and based on the detection of the p16 HPV-related protein. HPV-related OPSCC is very similar to HPV-related anogenital cancers in natural history, epidemiology, and pathophysiology. They both infect the stratified squamous epithelium, are sexually transmitted, and share the same risk factors in increased sexual partners, and the carcinogenic transformation of both are dependent on overexpression of HPV oncogenes E6 and E7.
HPV Prevalence in Head and Neck Cancer by Anatomical Site
The highest HPV detection rates occur in tonsil (53.9%) and base of the tongue (47.8%) among all sites of head and neck cancers. HPV 16 contributed to most HPV-positive cancers of the tonsils (93.8%), base of the tongue (97.9%), and soft palate (95.7%), and the relative contribution of HPV 16 was more than 50% in all sites. However, the oncogenic strains of HPV in OPSCC are lacking in Asia. HPV type 16 is the predominant strain detected in OPSCC in some reports from Asia. However, drawing from inference of HPV genotypes in cervical squamous cell carcinoma (SCC) in Asia-Pacific (APAC) countries where other oncogenic strains such as type 33, 41, 52, and 58 have been identified, the prevalence of these oncogenic strains and their significance in OPSCC in APAC needs further clarification.
p16 Testing
HPV-associated OPSCC is increasingly recognized and tested in all newly diagnosed OPSCC worldwide. As HPV 16 contributed to most HPV-related OPSCC, using p16 immunohistochemistry (IHC) as a surrogate for HPV detection for OPSCC has been established. p16 testing can be performed on fine needle aspiration (FNA) samples of cervical nodal metastases in cases of SCC of unknown origin. The clear separation of survivals is evident between p16-positive and p16-negative OPSCCs, indicating p16 testing’s value as a prognostic tool. Presently, p16 IHC testing is routinely performed for all OPSCC in the United States and only in eastern Asia, including Japan, Korea, and Taiwan, and in Singapore, Australia, and New Zealand.
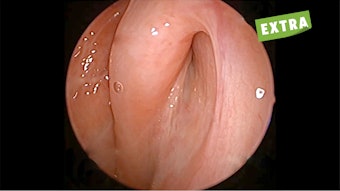
Of note, HPV-related precancerous lesions in the oropharynx have never been identified, and the primary tumor of HPV-related OPSCC is often small and sometimes occult. In this scenario, it is of particular importance to establish a biomarker to detect HPV-related oropharyngeal cancer at an early stage. At the University of Osaka, Tanaka et al. (2021) evaluated the diagnostic performance of HPV DNA and mRNA in oral gargle samples and circulating tumor HPV DNA (ctHPVDNA) in blood samples. The study found the sensitivity and specificity of oral HPV DNA, oral HPV mRNA, and ctHPVDNA were 82% and 100%, 85% and 94%, and 93% and 97%, respectively, for HPV-related OPSCC and were 20% and 100%, 0% and 100%, and 100% and 100%, respectively, for HPV-related cancer of unknown primary. ctHPVDNA correlated well with tumor burden and HPV copy number per tumor genome, whereas oral biomarkers did not. The authors conclude that ctHPVDNA is a promising biomarker for HPV-related OPSCC and cancer of unknown primary.
HPV Prevalence in Head and Neck Cancers
The U.S. Centers for Disease Control and Prevention (CDC) estimates that 70% of U.S. oropharyngeal cancer cases overall are probably caused by HPV. In Taiwan, with data from 528 cases of OPSCC, HPV positive (HPV DNA and/or p16 staining positive) was only detected in 150 cases (28.4%), though 82.8% were p16 positive. In Singapore, approximately 45% of OPSCC formalin-fixed, paraffin-embedded (FFPE) tumor samples were found to be p16 positive on immunohistochemistry (IHC).
The incidence of oropharyngeal cancer is increasing also in Japan. For instance, in Osaka Prefecture, the estimated crude incidence rate of oropharyngeal cancer increased significantly from 1.2 (1995) to 3.0 (2015) per 100,000 person-year in men and from 0.2 (1995) to 0.6 (2015) per 100,000 person-year in women.
Moreover, of oropharyngeal cancers treated at Osaka University Hospital, 38% and 68% were HPV-related during 1996 to 2009 and 2018 to 2021, respectively, indicating that the increase in oropharyngeal cancer is mostly attributed to the increase in the HPV-related one.
In a Taiwan population-based cohort study on the incidence trends of HPV-related head and neck cancer (HNC) in Taiwan using data from the Taiwan Cancer Registry from 1995 to 2009 found that the incidence of HPV-related HNC (1.3 per 100,000 in 1995 to 3.3 in 2009, annual percentage change [APC]=6.9, p=.0001) rose more rapidly than the incidence of HPV-unrelated HNC (from 10.4 to 21.7, APC=5.0, p=.0001).
However, the estimated HPV-attributed oropharynx cancer in Taiwan (men) is only 2.68 per 100,000 person-year in comparison with 8.5/100,000 in the U.S., which might indicate the incidence of HPV-related OPSCC is still rising in Taiwan. Unfortunately, HPV vaccination remains less common in APAC countries, and the incidence of HPV-related OPSCC is expected to further increase in the future in this region.
ASHNO Questionnaire Study on HPV-Related OPSCC
As a regional head and neck society, the Asian Society of Head and Neck Oncology (ASHNO) is committed to working to reduce the disease burden of HPV-related diseases, especially HPV-related HNC, by improving awareness, prevention, screening, and treatment for all genders in the APAC region.
ASHNO recently initiated a questionnaire on HPV-related OPSCC. ASHNO surveyed the impact of HPV screening and prevention—including the impact on the male population in each member country—and collected data from 14 APAC countries, which were divided into three different developing levels. There were 21 responders collected from 14 countries at different developing levels. The results indicated some important points.
In APAC countries:
- 76% have a national HPV screening program
- 91% have HPV vaccination, of which only 43% have a national program
- The vaccination program is provided mostly for women, none for men
- OPSCC incidence is higher for men than women, 3-4:1
- HPV-related OPSCC incidence shows more in developed countries, as high as 40%-50%
- HPV-related OPSCC incidence is parallel to development level
The survey indicated that in more developed countries, there is a higher incidence of HPV-related OPSCC, meaning countries with higher gross domestic product (GDP) growth, such as Japan, Korea, Singapore, and Taiwan, have higher incidence of HPV-related OPSCC. Lower resource countries have a lower incidence of HPV-related OPSCC.
The reasons behind these data could include the following:
- No routine HPV test. There is no regular HPV test established in some countries.
- Incidence ignored. The incidence of HPV-related OPSCC is low in some countries because the problem is just ignored. It is ignored particularly in male patients because there are no regular vaccination programs for men in this region.
- Culture or religion. Some populations are conservative or even suppressed sexually.
Treatment
HPV-related OPSCC is strongly associated with a favorable survival, while, conversely, HPV-negative OPSCC often flags a worse prognosis. The standard care for OPSCC is definitive chemoradiotherapy (CRT), even though surgical approaches followed by adjuvant radiotherapy/concurrent CRT have been proposed mostly in the APAC region.
Recent developments of robotic systems, such as the da Vinci® robot, have enabled surgeons to perform transoral robotic surgery (TORS) with greater ease and precision and with improved functional outcomes compared with open mandibulotomy approach. The role of mandibulotomy approach in HPV-associated OPSCC is hardly indicated nowadays. The safety, feasibility, and excellent oncologic outcomes following TORS have strengthened this surgical paradigm in treating OPSCC; TORS is increasingly adopted in APAC countries.
Finally, despite the increasing efforts to de-escalate treatments in HPV-positive OPSCC patients, most APAC centers have adopted a similar treatment philosophy in treating both HPV-positive and HPV-negative OPSCCs. Future studies are necessary to identify and select ideal HPV-associated OPSCC patients for de-escalation protocols using plasma HPV-DNA or other metabolic signatures.
Urgent Need in APAC
The following proposals can address the prevalence of OSPCC in APAC countries:
- HPV screening and vaccination programs, especially for men
- HPV-related OPSCC education and public awareness programs
- A study on the diagnosis (p16) and treatment results for HPV-related OPSCC in APAC countries