An Update on Noise-Induced Hearing Loss
The Hearing Committee provides an update on noise exposure limits and NIHL.
A. Morgan Selleck, MD, Hamid R. Djalilian, MD, and Isaac D. Erbele, MD, Hearing Committee members
Approximately 23 million Americans aged 20 and older suffer from noise-induced hearing loss (NIHL).1 NIHL is the most significant preventable cause of hearing loss in the United States.2 NIHL has traditionally been defined as occurring at 3, 4, or 6 kHz.3 It is determined by the severity and duration of the noise exposure as well as the underlying genetics of the individual. The prevalence of NIHL is higher with advanced age, the male gender, white (non-Hispanic) and Hispanic ethnicities, education level less than high school diploma, Mexico as country of birth, service in armed forces, smoking history, diabetes, and occupational and those with any kind of noise exposure.1 In economic terms, NIHL affects about 13% of the working population, with an estimated annual cost of $123 billion a year in the U.S.4
Recommended and Enforceable Noise Exposure Limits
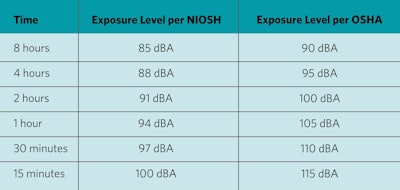
The Occupational Safety and Health Administration (OSHA) has established permissible noise exposure limits (PEL) for occupational noise exposure, which are enforceable by law. The National Institute for Occupational Safety and Health (NIOSH), the group responsible for studying NIHL, recommends slightly higher standards for their recommended exposure limits (REL). The two sets of limits are slightly different at the level, steps, and duration of exposure, but both standards are based on limiting the “dose” of noise individuals are exposed to in a given workday.
The exposure limits are based on A-weighted frequency response (dBA)—an average of sound intensity giving greatest weight to frequencies essential for speech. The OSHA PEL recommendations start at 90 dBA for an eight-hour time period. For every 5 dB increase in the average sound level, the permitted sound is reduced by half. This means under OSHA, a worker should only be exposed to 95 dbA sound for four hours, 100 dBA for two hours, etc.
The NIOSH REL starts at 85 dBA over an eight-hour period averaged over time. At this sound level over a lifetime of work, NIOSH estimates at least mild hearing loss in 14% of the population.5 For each 3 dB increase in the average sound intensity from there, the recommended duration of sound exposure is halved. Therefore, an 88 dBA sound is permitted for four hours, a 91 dBA sound for two hours, etc. Since the intensity of sound doubles with each increment of 3 dB, this exposes the individual to roughly the same noise dose; based on the physics of sound and the logarithmic decibel scale, 3dB increase is nearly equivalent in the doubling of the sound pressure. The table below shows the difference between the REL and PEL.
Table 1. The difference between recommended exposure limits and permissible noise exposure limits.
Therapies for Noise-Induced Hearing Loss
Therapy for NIHL consists of prevention and treatment. NIHL prevention techniques include education, workplace interventions, legislation, personal hearing protection devices (HPDs), and pharmacologic agents.6 Education through hearing loss prevention programs demonstrates some positive impact with improved use of HPDs, although overall has been disappointing in the prevention of hearing loss.6 Workplace interventions include upgrading equipment, creating physical barriers around loud sound sources, or isolating loud machines.6 Legislation changes have resulted in a 4.5 dBA decrease in noise levels in the mining industry, as well as downward trends in amount of noise exposure per year.7
Personal HPDs can prevent NIHL with an average noise exposure reduction of 20 dB.6,8-10 For a HPD to be effective, it must fit well, be comfortable, and be worn during the time of hazardous noise exposure. HPDs are rated based on their noise reduction rating (NRR), given in decibels of hearing reduction. The higher the NRR, the better hearing protection the device provides the user. NRR is calculated based on the degree of hearing protection when the device is properly fit. It indicates the level of reduction in decibels reaching a user’s inner ear for 98% of the population. NRRs for HPDs are generally 20s to low 30s in decibels, varying based on the type of HPD as well as the manufacturer. The following is a list of different types of HPDs:
- Premolded, Reusable Plugs
These ear plugs are made from silicone, plastic, or rubber. They commonly have multiple flanges and are sometimes referred to colloquially as “Christmas Tree” ear plugs. - Expandable Foam Plugs
Expandable foam plugs are made of a material that can be squeezed temporarily for insertion into the ear. Once in the ear, the plug expands to the shape of the ear canal. These plugs are inexpensive but may not fit every ear canal. - Earmuffs
Earmuffs are over-the-ear HPDs that form a seal around the ear on the outside to prevent noise intrusion into the ear canal. The primary advantage of these devices is that one size fits most individuals and can be worn in addition to ear plugs to provide double hearing protection. - Active (Electronic/Noise Cancellation) Earmuffs
Electronic earmuffs work similarly to earmuffs in that they block sound from entering the ear by creating an airtight seal around the auricle. These devices perform best for reducing constant loud noise, for example, engines. - Selective Attenuation Earplugs
Selective attenuation ear plugs are intended for use around impulse noise. These earplugs are also called nonlinear, level-dependent, or impulse earplugs. They are designed to allow low-amplitude sound—e.g., speech, command, ambient sound—and block loud impulse sound such as gun fire or explosion.
HPD effectiveness is predicated on correct and consistent utilization, which in practice is an infrequent occurrence.11-15 This led to interest in prevention of NIHL through pharmacologic agents. The underlying mechanism of NIHL is thought to be free radical species damaging outer cochlear hair cells. Medications target that proposed etiology through removal of free radicals, changing oxygen delivery, improving the integrity of the cochlear hair cells, or repairing the vascular endothelium.16 Medications that have been studied include alpha-lipoic acid (ALA), oxygen, beta-carotene, carbogen (5% carbon dioxide, 95% oxygen), ebselen, Mg-asparate, N-acetylcysteine (NAC), and vitamins C, E, and B12.16 Data are limited on the efficacy of these medications, and while some medications (Mg-aspartate, carbogen, vitamin B12, NAC, and ALA) appear promising with statistically significant effects, there is currently no medication with an Food and Drug Administration (FDA)-approved indication for NIHL or a current recommendation for pharmaceutical prophylaxis.16,17
Treatment of acute-onset NIHL (aNIHL) consists primarily of steroids and hyperbaric oxygen therapy treatment, although other medications including vasodilators, antioxidants, nootropics (cognitive enhancers), and cell apoptosis inhibitors have been studied.18,19 Improvement in aNIHL has been associated with treatment within 48 hours of the acoustic trauma, patients with high-frequency hearing loss, and those that also received treatment with a nootropic agent.18 Steroids have also demonstrated to improve hearing thresholds, both low and high frequency, in those with aNIHL.19 Studies are heterogenous and lack consistency, necessitating additional future research to better understand the impact of these treatment modalities.
Future Directions for Noise-Induced Hearing Loss
Despite what we know about NIHL, significant gaps in our understanding remain. In particular, the precise relationship between temporary and permanent threshold shifts remains unknown and predicting who will develop permanent hearing loss from aNIHL remains unclear. Also, most models used to understand NIHL are limited, either relying on small animals with poor frequency overlap with humans or on temporal bone histology collected decades after the noise insult.
There are several promising leads to explore NIHL, however. Over the past decade, several groups have been working with human-induced pluripotent cells to develop otic organoids—3D tissue cultures that mimic tissue of the inner ear.20 This work combined with organ-on-a-chip technology may allow studies on human tissue to help solve some of the difficulties with inadequate models. Additionally, large animals like sheep resemble the human auditory system more closely than rodents, and they may provide a better model to study, though the cost of using this animal model is much higher.21,22 Concurrently, there is work in using microneedles through the round window membrane to allow safe removal of endolymph or drug delivery,23 mitochondrial function enhancement,24 and hair cell regeneration continues to be an area of active study.25
Conclusion
NIHL continues to be a common, irreversible cause of sensorineural loss. Hearing protection by avoiding noise and wearing well-fitting personal hearing protective devices remains the best way to prevent NIHL. Although more study is needed for therapeutics for aNIHL, steroids, nootropics, and hyperbaric oxygen may be reasonable treatments. Improved understanding of the mechanisms of NIHL may allow further exploration into additional therapies.
Department of Defense Disclosure: The views expressed herein are those of the author(s) and do not necessarily reflect the official policy or position of the Defense Health Agency, Brooke Army Medical Center, the Department of Defense, nor any agencies under the U.S. Government.
Conflicts of interest: None
References
- Mahboubi H, Zardouz S, Oliaei S, Pan D, Bazargan M, Djalilian HR. Noise-induced hearing threshold shift among US adults and implications for noise-induced hearing loss: National Health and Nutrition Examination Surveys. Eur Arch Otorhinolaryngol. 2013;270(2):461-467.
- Bronzaft AL. Noise: combating a ubiquitous and hazardous pollutant. Noise Health. 2000;2(6):1-8.
- Coles RR, Lutman ME, Buffin JT. Guidelines on the diagnosis of noise-induced hearing loss for medicolegal purposes. Clin Otolaryngol Allied Sci. 2000;25(4):264-273.
- Neitzel RL, Swinburn TK, Hammer MS, Eisenberg D. Economic impact of hearing loss and reduction of noise-induced hearing loss in the United States. J Speech Lang Hear Res. 2017;60(1):182-189.
- National Institute for Occupational Safety and Health. Criteria for a recommended standard: occupational noise exposure, revised criteria 1998. https://www.cdc.gov/niosh/docs/98-126/
- Tikka C, Verbeek JH, Kateman E, Morata TC, Dreschler WA, Ferrite S. Interventions to prevent occupational noise-induced hearing loss. Cochrane Database Syst Rev. 2017;7(7):Cd006396.
- Joy GJ, Middendorf PJ. Noise exposure and hearing conservation in U.S. coal mines—a surveillance report. J Occup Environ Hyg. 2007;4(1):26-35.
- Hong O. Hearing loss among operating engineers in American construction industry. Int Arch Occup Environ Health. 2005;78(7):565-574.
- Brink LL, Talbott EO, Burks JA, Palmer CV. Changes over time in audiometric thresholds in a group of automobile stamping and assembly workers with a hearing conservation program. AIHA J (Fairfax, Va). 2002;63(4):482-487.
- Hessel PA. Hearing loss among construction workers in Edmonton, Alberta, Canada. J Occup Environ Med. 2000;42(1):57-63.
- Neitzel R, Seixas N. The effectiveness of hearing protection among construction workers. J Occup Environ Hyg. 2005;2(4):227-238.
- Hong O, Ronis DL, Lusk SL, Kee GS. Efficacy of a computer-based hearing test and tailored hearing protection intervention. Int J Behav Med. 2006;13(4):304-314.
- Kerr MJ, Savik K, Monsen KA, Lusk SL. Effectiveness of computer-based tailoring versus targeting to promote use of hearing protection. Can J Nurs Res. 2007;39(1):80-97.
- McCullagh M, Lusk SL, Ronis DL. Factors influencing use of hearing protection among farmers: a test of the pender health promotion model. Nurs Res. 2002;51(1):33-39.
- Hong O, Chin DL, Ronis DL. Predictors of hearing protection behavior among firefighters in the United States. Int J Behav Med. 2013;20(1):121-130.
- Gupta A, Koochakzadeh S, Nguyen SA, Brennan EA, Meyer TA, Lambert PR. Pharmacological prevention of noise-induced hearing Loss: a systematic review. Otol Neurotol. 2021;42(1):2-9.
- Chang PH, Liu CW, Hung SH, Kang YN. Effect of N-acetyl-cysteine in prevention of noise-induced hearing loss: a systematic review and meta-analysis of randomized controlled trials. Arch Med Sci. 2022;18(6):1535-1541.
- Koochakzadeh S, Gupta A, Nguyen SA, et al. Hearing outcomes of treatment for acute noise-induced hearing loss: a systematic review and meta-analysis. Otol Neurotol. 2020;41(8):e971-e981.
- Ahmed MM, Allard RJ, Esquivel CR. Noise-induced hearing loss treatment: systematic review and meta-analysis. Mil Med. 2022;187(5-6):e661-e666.
- Nist-Lund C, Kim J, Koehler KR. Advancements in inner ear development, regeneration, and repair through otic organoids. Curr Opin Genet Dev. 2022;76:101954.
- Heffner H, Heffner R. Auditory perception. Behaviour. 1992;24:81.
- Péus D, Dobrev I, Prochazka L, et al. Sheep as a large animal ear model: middle-ear ossicular velocities and intracochlear sound pressure. Hear Res. 2017;351:88-97.
- Aksit A, Rastogi S, Nadal ML, et al. Drug delivery device for the inner ear: ultra-sharp fully metallic microneedles. Drug Deliv Transl Res. 2021;11(1):214-226.
- Okur MN, Djalilian HR. Approaches to mitigate mitochondrial dysfunction in sensorineural hearing loss. Ann Biomed Eng. 2022 Dec;50(12):1762-1770.
- McLean WJ, Hinton AS, Herby JTJ, et al. Improved speech intelligibility in subjects with stable sensorineural hearing loss following intratympanic dosing of FX-322 in a phase 1b study. Otol Neurotol. 2021;42(7).