Are Alginates All That?
A discussion of traditional and alternative therapies in the management of gastroesophageal reflux disease (GERD).
Mark R. Gilbert, MD, Voice Committee member

What was 50 years ago a disease in the purview solely of gastroenterologists, gastroesophageal reflux disease (GERD) is now a bread and butter diagnosis for otolaryngologists. GERD is estimated to astonishingly affect up to 20% of adults.1 First-line therapy of GERD is proton pump inhibitor therapy (PPI), which are some of the most prescribed pharmaceuticals in the world. In concert with the growth of acid reflux awareness, the market continues to grow. By 2031, the global PPI market is projected to reach $5.64 billion, with compounded annual growth of 4.2%.2 However, PPIs are not benign therapy, and thus have specific indications from gastroenterologists. American Gastroenterology Association (AGA) clinical practice guidelines recommend that patients with Barrett’s esophagus or symptomatic GERD should take a long-term PPI, but the dosage should periodically be re-evaluated to the lowest effective dosage.3 They also report that patients with uncomplicated GERD who respond to short PPIs should attempt to stop or reduce them, or should commit to ambulatory pH/impedance testing before staying on their use for life.
The reason for these recommendations is the association of PPIs with several side effects. An AGA review of the risks and benefits of PPI therapy from 2017 indicated several conditions that have been associated with PPI usage, including acute kidney injury and chronic kidney disease, dementia, bone fractures, myocardial infarction, small intestinal bacterial overgrowth, spontaneous bacterial peritonitis, Clostridium difficile infection, pneumonia, micronutrient deficiencies, and gastrointestinal malignancies.3 However, all these associations were considered to have low or very low evidence. Despite this lack of good evidence, concerns persist, and data grows regularly. The COGENT study in 2010 showed that PPIs do not have a meaningful reaction with Clopidogrel (Plavix), but pharmaceutical websites like GoodRx still list this as a possible interaction in which there is reduction in antiplatelet activity of Clopidogrel. A recent literature review showed an association with PPI usage and an increase in gastric cancer risk.4 A large meta-analysis in 2022 showed no association between PPI usage and dementia, but two large studies in 2023 disagreed, showing an increased risk with prolonged usage (>4.4 years) in one and with an increased rate ratio with longer usage in another.5-7
Also, the U.S. Food and Drug Administration (FDA) has several class warnings on possible effects of PPI usage, including hypomagnesemia, interstitial nephritis, and B12 deficiency.8 Finally, in 2022, an Iranian study showed that PPI users were more symptomatic and had higher COVID-19 severity than non-users, with a nonsignificant trend toward higher mortality.9
H2-receptor antagonists (i.e., H2 blockers), another class of acid secretory therapy, have had their own problems. Ranitidine was taken off the market in 2019 due to discovery of the likely breakdown of the active pharmaceutical ingredient to N-nitrosodimethylamine (NDMA), a possible carcinogen.10 H2 blockers have also been associated with rapid tachyphylaxis (i.e., tolerance), even by the second day, with symptom relief possibly due to desensitization of the esophagus to acid, which may provide false security.11
These problems have even more relevance when it is considered how many patients are treated with PPIs or H2 blockers for laryngopharyngeal reflux disease (LPRD) but are managed by otolaryngologists because they do not meet the definition of complicated GERD. Do they even need to be on antisecretory at all and is there another way to manage LPRD symptoms? Is there another way to physically prevent reflux besides surgical interventions? This brings us to the novel approach of alginate therapy, a growing area of reflux management.
Maybe Alginates Are the Panacea?
Steven Sims, MD, recalls first treating occasional patients with commercial alginate (chewable Gaviscon Advance) for symptomatic reflux disease several years ago. Dr. Sims, who is a professor of otolaryngology—head and neck surgery and director of the Chicago Institute for Voice Care at the University of Illinois-Chicago, said when his patients began to notice their morning heartburn symptoms improving with the supplement, he thought there was something different about this product.
“That was probably the first group of patients who made me think, ‘there’s something to this alginate—the mechanical inhibition of the reflux helps with a lot of the symptoms that people were experiencing or complaining about even more than acid suppression,’” he said.
Alginate-based pharmaceuticals have been used for GERD in Europe for decades. They occur naturally in brown algae (i.e., seaweed) as a structural polysaccharide, and they are found in many different seaweed species in the world.12 However the most effective pharmaceuticals are produced from the stems of Laminaria hyperborea found predominately in the ocean around Norway due to a high concentration of polysaccharide chains with blocks of repeating α-L-guluronic acid that bind divalent metal cations such as Ca2+. When combined with sodium bicarbonate and calcium carbonate and exposed to the acidic gastric environment, these polysaccharides form a strong buoyant raft of alginate that is coherent, uniform, and floats just below the liquid surface.
Alginates have been shown in vitro and in vivo to act in several ways that contribute to the treatment of the sequalae of acid reflux.12,13 Primarily they act as a physical barrier to gastric acid entry into the esophagus by floating on top of the stomach contents that may reflux. They further displace the postprandial highly acidic “acid pocket” that forms just below the gastroesophageal junction, thereby reducing postprandial reflux. They have been shown to remove both pepsin and bile acids from gastric reflux, which is important as pepsin is responsible for esophageal barrier dysfunction by low pH stomach acid.12,13 Alginates have also been shown to act as a topical protectant of esophageal mucosa by bioadhesive properties, and they have been shown in vitro to protect against pepsin-acid induced esophageal barrier disruption.13
Sodium alginate research has grown tremendously in the past few years. A Pubmed search of “alginate” and “reflux” shows nearly half of all the published literature has been published in the past ten years. (Figure 1)
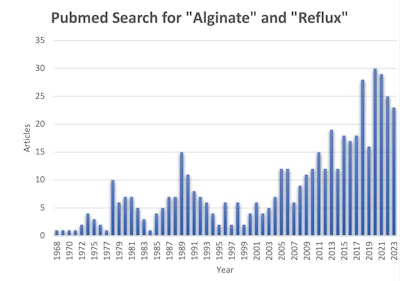 Figure 1. Pubmed Search for "Alginate" and "Reflux."
Figure 1. Pubmed Search for "Alginate" and "Reflux."
Recent clinical literature has established that alginates have very practical uses in patients with reflux disease. A meta-analysis in 2017 showed that alginate therapy provides superior benefit over placebo and antacids in treating GERD symptoms and traditional therapies were only slightly favored over alginates and not significantly.14 Most recently, a randomized clinical trial conducted in 2023 showed that alginates are effective in managing rebound reflux symptoms when washing out PPI before manometry and impedance therapy, suggesting that alginates could be effective for rebound symptoms in effective weaning of PPI therapy.15 This usage may have very practical applications as many patients who were empirically trialed on extended PPI therapy may be on therapy for years due to rebound effects. These patients may suffer from side effects of PPI therapy needlessly and could be weaned if an extended course of alginate therapy were instituted.
Alginates achieve a more rapid reduction in acid exposure than PPI or H2 blockers.12 Alginates have also additional uses in unique patient populations as they have demonstrated no safety concerns in children or in pregnant patients and in fact have been recommended as first-line medical therapy for pregnant or breastfeeding patients.16 In contrast, PPIs are category B or C drugs in pregnant or breastfeeding patients. Still, in general, no clear studies have analyzed alginates for maintenance therapy for GERD, and there is limited data on whether continuous treatment improves quality of life or other measures.12
ENTrepeneurs Develop Their Own Formulations
Peter C. Belafsky, MD, MPH, professor of otolaryngology and director of the Center for Voice & Swallowing at UC Davis, was in fellowship with Jamie Koufman, MD, at Wake Forest when he was first made aware of alginate therapy. He cites the research of Peter W. Dettmar, PhD, a mentor who at the time was at Reckitt Benckiser, the company who marketed the primary commercial alginate product in Europe, Gaviscon Advance.
“At the time, we were using it primarily as an adjunct to antisecretory therapy, whether it be PPI or H2 blockers,” said Dr. Belafsky. “We used to look at PPIs as giving out skittles,” he contrasts, “But in my career it seems like I’ve spent more effort trying to get people off PPIs and put them on alginates, along with lifestyle and diet, to try and get people off the drugs rather than use it as an adjunct to drugs.”
Ramon S. Franco, MD, associate professor of otolaryngology-head and neck surgery and medical director of the voice and speech laboratory at Massachusetts Eye and Ear, had a similar experience.
“For all these years, [we were] giving people PPIs. I started my fellowship in 2000, and literally every person that walked into our clinic left with a Prilosec or Nexium prescription. And back then we were instantly doing 40 BID. Sometimes my mentor would give people TID dosing of 40mg. And I just kept thinking reflux is not acid, right? Those are two separate things. Refluxing is just the actual movement. This medicine doesn’t stop any of the movement, [it doesn’t prevent] the stuff from the stomach [getting] into the esophagus.”
A little over a decade later, Dr. Franco and Dr. Belafsky formed their own alginate supplement product and company, Reflux Gourmet.® Dr. Belafsky reports he has been amazed by the success of the therapy,
“I’m really just blown away by how many people we’ve been able to help,” he said. “We’ve been doubling our sales every year.”
James J. Daniero, MD, associate professor of otolaryngology—head and neck surgery at the University of Virginia School of Medicine and director of the division of laryngology, similarly researched his own alginate product for several years before it was debuted last year as RefluxRaft.® He stated his interest grew out of his patients’ and his own experiences.
“Patients were always asking about how to avoid PPI use due to increased awareness of side effects, and others were symptomatic from nonacidic reflux with no options other than behavioral change available. I went looking for options to help these patients and learned how Europe has had treatments for nonacid reflux since the 1970s. There was actually good evidence supporting alginate therapy, and I didn’t see much downside, so it was a no-brainer. I have acid reflux and started taking it myself. I was concerned about possible connection of PPIs with dementia, so I transitioned off a PPI to alginate with success.”
PPI Versus Alginate
No one is suggesting that PPI therapy is not necessary, however. Michael Vaezi, MD, PhD, MSc (Epi), professor of medicine, director the Center for Swallowing and Esophageal Disorders, and clinical director of the division of Gastroenterology at Vanderbilt University School of Medicine, does not use alginates routinely in his practice.
“I usually do not recommend [alginate] as first-line—PPIs are first and then if no benefit, I may consider,” he said. Good candidates are, “Those that have failed original attempts with PPIs and H2 receptor antagonists.”
However in his complex gastroenterology practice, he has mixed success with alginates. “Those who do not respond to PPIs are also less likely to respond to alginates,” he said.
Dr. Belafsky agrees. “The people that have complicated GERD, whether it’s metaplasia, stricture, dysplasia, hiatal hernia, ineffective motility—those patients really need aggressive acid suppression. But that’s a small minority of the patients we see; the majority have what we consider endoscopy negative reflux disease, and that’s where we like to use the alginates as first-line.”
William Z. Gao, MD, co-director of the University of Chicago Medicine Voice & Swallowing Center, recommends lifestyle changes for reflux instead of acid suppression.
“My belief is that dietary/lifestyle elements are critical—appropriate lifestyle counseling is first and foremost,” he said. “But if there’s an absence of GERD symptoms like heartburn or substernal symptoms that are more classically associated with GERD, then I don’t recommend any type of acid suppression as first-line treatment. We’ll add a PPI typically if there are only partial responses, but the majority of LPR tends to be either nonacidic or weakly acidic.”
As for patients that he considers for alginate therapy, Dr. Gao said, “Any patient who primarily presents with more LPR specific symptoms—throat clearing, mucus in the throat, globus sensation, reflux leading to mild dysphonia, chronic cough. And we would recommend that either alone or in combination with PPI. I recommend using it initially as much as possible—after meals and before bed with a wedge pillow, which later can be tapered after symptom improvement.”
Dr. Gao said he finds that alginates help establish the etiology in some cough patients.
“I think chronic cough patients who seem to have the primary driver of their cough related to reflux are great candidates for alginates as a trial, especially if they have a known hiatal hernia,” he said. “What I find is that if they use alginates and the cough is clearly controlled with use, then that provides evidence it is reflux related and may benefit from surgical management.”
Dr. Sims recommends alginate therapy when patients express hesitance in PPI therapy or are trying to avoid medication.
“Particularly when working with performers, a lot of them don’t necessarily want to take a traditional pharmaceutical. So when the patient says they don’t want to take those medicines, or they’ve heard something about it, or they’re worried about the side effects, I can offer other things.” He also feels older patients make good candidates, “Just because of some of the known side effects with calcium and magnesium metabolism and potential increased risk of fractures and osteopenia.”
Not the End-All Be-All
Candace Hrelec, MD, a laryngologist in private practice in Sarasota, Florida, learned about alginates while in her residency during her laryngology rotation.
“We were having to have the patients buy it through Gaviscon Advance UK, and it always interested me because it was something different, and there wasn’t a lot about it in U.S. literature at that time and not a lot of marketing on it in the United States.
“I try to gauge the patient’s interests, needs, and wants. I’ve used more alginates recently for getting patients off PPIs and H2 blockers.” However, she noted that the cost can be prohibitive for some patients and, “A lot of my patients are older and don’t know how to use Amazon to get the medication. It’s not available over-the-counter, and I think that’s where I’ve had more issues. Some people will tend to say it’s a little bit too expensive for just one bottle for the month, they don’t like the taste, or it’s just not worked as effectively as some of the PPIs and H2 blockers.”
However, she said, “It’s a healthier alternative, especially when people fear PPIs or H2 blockers, and it’s safe in pregnant women, and it’s safe in infants. I think it really clicks in their head when you say that.”
Regarding future alginate product availability and cost, Dr. Sims is optimistic. “The fact that there are [different alginate products] is encouraging that as perhaps there is more demand, there will be more companies who are able to help [the] supply and that will eventually start driving the price down. I think it is encouraging.”
Dr. Daniero thinks the alginate market will continue to grow.
“Awareness of alginate therapy has been growing. Patients are looking for more natural solutions, and the result is a natural shift in the market. There are now at least eight alginate products on the market,” he said.
Dr. Franco agrees, “There have been some formulations out there for a little while now. You can buy regular sodium alginate and you can make up your own stuff. But it’s a matter of making it palatable and then how do you preserve it because it’s a high pH product, it’s a thick liquid, and not a lot of places have expertise with creating it and then packaging it. But I do think that the space is growing.”
Other Natural Alternatives?
There are still other therapies in nature, and a variety of other natural products may, to coin a phrase, uproot the excitement around alginate therapy. Turmeric (i.e., curcumin) has been shown in a recent clinical trial to be significantly superior in managing dyspepsia symptoms and in treating H. pylori when combined with famotidine than when compared with famotidine alone.17 Following this, a randomized, double anonymized clinical trial conducted in 2023 showed turmeric had comparable efficacy to omeprazole in treating functional dyspepsia.18
Dr. Sims has also occasionally recommended other alternative therapies, including, “Iberogast, deglycyrrhizinated licorice root, esophageal guardian, and apple cider vinegar (as a prokinetic agent). A lot of this is the concept that what we’re calling reflux really has a lot of components to it.”
Future of Reflux Therapy
What is the future of reflux therapy? Acid suppression or natural alternatives, or both? Dr. Sims thinks it is in the determination of precisely what kind of reflux a patient has.
“Some of this will be rooted in our understanding of reflux,” he said. “This umbrella of reflux, we need to come up with some phenotypes. What kind of reflux are we talking about and then begin tailoring the therapy for that. I think there are some patients for whom a daily PPI probably is the appropriate management because they do have hypersecretion of acid, and I think there will be a lot of people for whom alginates are going to be a great option.”
Dr. Gao agrees, “I don’t think it’s a matter of alternative versus not. I think it’s a matter of what are we treating and are we treating it most appropriately? I think PPIs and H2 blockers will always be part of the picture and part of the necessary treatment paradigm. It’s just a matter of understanding what is the more effective and efficient triage of treatment.”
References
- El-Serag HB, Sweet S, Winchester CC, Dent J. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. Jun 2014;63(6):871-80. doi:10.1136/gutjnl-2012-304269
- Proton Pump Inhibitors Market Size to Surpass US$ 5.64 Billion by 2031 - Growth Plus Reports. Yahoo! Finance. 2023. Accessed 11/9/2023, 2023. https://finance.yahoo.com/news/proton-pump-inhibitors-market-size-123000129.html?soc_src=social-sh&soc_trk=ma
- Freedberg DE, Kim LS, Yang YX. The Risks and Benefits of Long-term Use of Proton Pump Inhibitors: Expert Review and Best Practice Advice From the American Gastroenterological Association. Gastroenterology. Mar 2017;152(4):706-715. doi:10.1053/j.gastro.2017.01.031
- Abbas MK, Zaidi ARZ, Robert CA, Thiha S, Malik BH. The Safety of Long-term Daily Usage of a Proton Pump Inhibitor: A Literature Review. Cureus. Sep 4 2019;11(9):e5563. doi:10.7759/cureus.5563
- Northuis CA, Bell EJ, Lutsey PL, et al. Cumulative Use of Proton Pump Inhibitors and Risk of Dementia: The Atherosclerosis Risk in Communities Study. Neurology. Oct 31 2023;101(18):e1771-e1778. doi:10.1212/WNL.0000000000207747
- Pourhadi N, Janbek J, Jensen-Dahm C, Gasse C, Laursen TM, Waldemar G. Proton pump inhibitors and dementia: A nationwide population-based study. Alzheimers Dement. Oct 5 2023;doi:10.1002/alz.13477
- Ahn N, Nolde M, Krause E, et al. Do proton pump inhibitors increase the risk of dementia? A systematic review, meta-analysis and bias analysis. Br J Clin Pharmacol. Feb 2023;89(2):602-616. doi:10.1111/bcp.15583
- Strand DS, Kim D, Peura DA. 25 Years of Proton Pump Inhibitors: A Comprehensive Review. Gut Liver. Jan 15 2017;11(1):27-37. doi:10.5009/gnl15502
- Shokri MA, Moghadam Fard T, Ramim T, Hejrati A, Hejrati L, Mokhtare M. What is the role of proton pump inhibitors consumption on the clinical presentation and severity of COVID-19 infection? Ann Pharm Fr. Mar 2023;81(2):210-219. doi:10.1016/j.pharma.2022.08.013
- Aldawsari FS, Alshehry YM, Alghamdi TS. N-nitrosodimethylamine (NDMA) contamination of ranitidine products: A review of recent findings. J Food Drug Anal. Mar 15 2021;29(1):39-45. doi:10.38212/2224-6614.1133
- McRorie JW, Kirby JA, Miner PB. Histamine2-receptor antagonists: Rapid development of tachyphylaxis with repeat dosing. World J Gastrointest Pharmacol Ther. May 6 2014;5(2):57-62. doi:10.4292/wjgpt.v5.i2.57
- Bor S, Kalkan IH, Celebi A, et al. Alginates: From the ocean to gastroesophageal reflux disease treatment. Turk J Gastroenterol. Sep 2019;30(Suppl2):109-136. doi:10.5152/tjg.2019.19677
- Samuels TL, Yan K, Patel N, et al. Alginates for Protection Against Pepsin-Acid Induced Aerodigestive Epithelial Barrier Disruption. Laryngoscope. Dec 2022;132(12):2327-2334. doi:10.1002/lary.30087
- Leiman DA, Riff BP, Morgan S, et al. Alginate therapy is effective treatment for GERD symptoms: a systematic review and meta-analysis. Dis Esophagus. May 1 2017;30(5):1-9. doi:10.1093/dote/dow020
- Vales A, Coyle C, Plehhova K, Hobson A, Woodland P. Randomised clinical trial: the use of alginates during preinvestigation proton pump inhibitor wash-out and their impact on compliance and symptom burden. BMJ Open Gastroenterol. Jan 2023;10(1)doi:10.1136/bmjgast-2022-001026
- Thelin CS, Richter JE. Review article: the management of heartburn during pregnancy and lactation. Aliment Pharmacol Ther. Feb 2020;51(4):421-434. doi:10.1111/apt.15611
- Panahi Y, Karbasi A, Valizadegan G, et al. Effect of Curcumin on Severity of Functional Dyspepsia: a Triple Blinded Clinical Trial. Adv Exp Med Biol. 2021;1308:119-126. doi:10.1007/978-3-030-64872-5_10
- Kongkam P, Khongkha W, Lopimpisuth C, et al. Curcumin and proton pump inhibitors for functional dyspepsia: a randomised, double blind controlled trial. BMJ Evid Based Med. Sep 11 2023;doi:10.1136/bmjebm-2022-112231