Pearls from Beyond the Textbook: Mohs Reconstruction
The creative and individualizing challenge we face is to reconstruct not just tissue, but the personal and defining visage of a human being.
Bonnie Chen, MD, and C.W. David Chang, MD, members of the Facial Plastic and Reconstructive Surgery Education Committee
Reconstruction of facial defects is a surgically interesting challenge. Picking the right reconstruction plan is a balance of reconstruction fidelity, cosmesis, and function. While we cognitively create a hierarchy of options via the reconstruction ladder, we often dogmatically dismiss the lower rungs of the ladder when dealing with defects involving the complex contours of the nose and lips. However, fully exploring shared decision-making—marrying medical advice and the patient’s values and preferences—may lead to consideration of plans that buck the “textbook” method.
“Some patients might not be mentally or psychologically prepared for more complicated options,” says Matthew K. Lee, MD, Cedars-Sinai Medical Center. “In those situations, we should simplify the treatment plan to make the patient feel more at ease and to meet them in their comfort zone.”
Keeping it simple: the power of primary closure
For large nasal tip defects > 2.5 cm in size, surgeons tend to lean toward the paramedian forehead flap for cutaneous coverage. However, executing such an option requires the patient to accept extra wound care or a prolonged recovery time, given the multistage nature of the reconstruction. Careful analysis of the patient’s anatomy and anticipation of reconstructive consequences could lead to considering primary closure as a viable option. “Reconstructive maneuvers can induce secondary deformities, such as rotating or narrowing the tip, which can be utilized to a patient's benefit.” notes G. Nina Lu, MD, University of Washington. In a patient with a larger nasal tip and tip ptosis, wide undermining of surrounding tissue with primary closure may yield an excellent aesthetic outcome (Figures 1 and 2).
 Figure 1. Nasal tip and dorsum defect closed primarily along its narrowest width. Primary closure is used here to create a narrow a wide nasal tip.
Figure 1. Nasal tip and dorsum defect closed primarily along its narrowest width. Primary closure is used here to create a narrow a wide nasal tip.
 Figure 2. Nasal tip defect closed primarily superior-inferiorly. This technique requires wide undermining and is useful in patients with underlying tip ptosis.
Figure 2. Nasal tip defect closed primarily superior-inferiorly. This technique requires wide undermining and is useful in patients with underlying tip ptosis.
In Lieu of Two-Stage Interpolated Flaps
Large defects of the nasal ala—and especially those abutting the nostril rim—are commonly reconstructed with a melo-labial flap or paramedian forehead flap. However, for a highly visible patient such as a schoolteacher, a multistage procedure with a pedicled trunk may not be a practical or acceptable reconstruction plan. As a compromise, a full thickness supraclavicular skin graft can provide a one-stage procedure with satisfactory cosmesis (Figure 3). While alar notching should be an anticipated potential secondary consequence, additional small touch-up procedures could be later pursued. Imperfect reconstructive strategies can be performed, explains Nikita Gupta, MD, University of Kentucky, “with the understanding that the textbook answer is still available as a backup revision option.” Auricular composite grafts can also be utilized, providing soft tissue coverage while maintaining ala structural rigidity and aesthetic form (Figure 4). Composite grafts are often underutilized because of their reportedly high failure rates secondary to higher metabolic requirements for survival. Circumspect selection may partially ameliorate concerns if surgeons remain wary of patients with current tobacco use, diabetes, bleeding disorders, thyroid disease, nutritional deficiencies, history of radiation, or poor peri-defect microcirculation. Delayed reconstruction (> 6 days) may also improve graft success by improving surgical bed vascularity.
 Figure 3. A full thickness skin graft from the supraclavicular region was used to reconstruct this nasal ala defect. It would also be reasonable to consider placing an alar rim graft to prevent alar notching given the defect's proximity to the alar rim.
Figure 3. A full thickness skin graft from the supraclavicular region was used to reconstruct this nasal ala defect. It would also be reasonable to consider placing an alar rim graft to prevent alar notching given the defect's proximity to the alar rim.
 Figure 4. An auricular composite graft was used to reconstruct a partial thickness nasal ala defect abutting the nostril margin. Composite grafts may be useful for defects < 1.5 cm.
Figure 4. An auricular composite graft was used to reconstruct a partial thickness nasal ala defect abutting the nostril margin. Composite grafts may be useful for defects < 1.5 cm.
Lip Reconstruction: Beyond Karapandzic and Cross-Lip Flaps
The lip consists of skin, muscle, and mucosa. Reconstruction requires maintaining the sphincteric function that maintains oral competence as well as reestablishing the vermilion, color, and bulk of the lips. For central lower lip cutaneous defects spanning > 2/3 of the vermilion, larger procedures such as a Karapandzic flap or transposing additional tissue from the cheek (e.g., Gilles, Bernard-Burow methods) are typically considered. However, commonly the lip defect post-Mohs appears larger than what was actually lost due to retraction of the margins. Surprisingly, often a cutaneous wedge resection and W-plasty can achieve closure. Overlapping or imbricating the orbicularis oris muscle at the margin may reduce the loss of lip bulk that can occur with closure tension (Figure 5). An alternative to re-establishing bulk of a partial thickness cutaneous lateral red lip defect is utilizing the facial artery musculomucosal flap with the inclusion of the buccinator muscle within the flap (Figure 6).
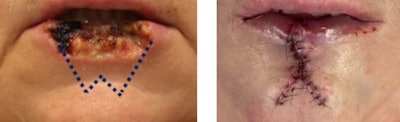 Figure 5. Lower lip cutaneous defect reconstructed with a wedge resection, W plasty, and imbrication of the orbicularis oris muscle to provide additional lip fullness.
Figure 5. Lower lip cutaneous defect reconstructed with a wedge resection, W plasty, and imbrication of the orbicularis oris muscle to provide additional lip fullness.
 Figure 6. Lower lip cutaneous defect reconstructed with a FAMM flap. The addition of the buccinator muscle within the flap adds bulk to the lip.
Figure 6. Lower lip cutaneous defect reconstructed with a FAMM flap. The addition of the buccinator muscle within the flap adds bulk to the lip.
“The most aesthetic reconstructive surgical option may not always be the best for the patient,” opines Andrea M. Park, MD, University of California, San Francisco. “It's important to listen to what the patient wants and work together to find an option that meets the patient's goals [and] expectations." That’s the creative and individualizing challenge we face when we reconstruct not just tissue, but the personal and defining visage of a human being.
References
Baker SR. Local Flaps in Facial Reconstruction, 4th Edition. 2022.
Yamasaki A, Dermody SM, Moyer JS. Reducing risks of graft failure for composite skin-cartilage grafts. Facial Plast Surg Clin North Am. 2023;31(2):289-296. doi:10.1016/j.fsc.2023.01.007
Duranceau M, Ayad T. The facial artery musculomucosal flap: Modification of the harvesting technique for a single-stage procedure. Laryngoscope. 2011;121(12):2586-2589. doi:10.1002/lary.22343