Current Management of Pediatric Facial Fractures
Many pediatric fractures do not require operative intervention.
Nikita Gupta, MD, Lauren A. Bohm, MD, Brianne Barnett Roby, MD, and Jonathan Lee, MD
The presentation of pediatric facial fractures differs from that in adults due to effects of developmental anatomy as well as different fracture patterns. Varying cranial-to-facial ratios, sinus pneumatization, bone compliance, and developing dentition cause these distinctions. This article discusses the management strategies for nasal bone, orbital floor, zygomaticomaxillary, and mandible fracture patterns.
Nasal trauma is commonly seen in the pediatric group with more bony trauma seen with increased facial growth. When addressing cartilaginous trauma to the septum, preservation of growth plates prior to puberty is key. The sphenodorsal and sphenospinal zones affect the length and height of the dorsum and forward outgrowth of the premaxilla, respectively, and are located at the bony-cartilaginous junction. Disruption can cause underdevelopment in vertical height and sagittal projection of the nose, so septal resection is avoided, when possible, in favor of repositioning in young patients.
In orbital floor fractures, a trapdoor type is more often encountered in the pediatric population. Considerations for surgery include extraocular muscle entrapment, enophthalmos, and/or hypoglobus. Better outcomes have been found in the pediatric population when addressed within two weeks of injury due to better extraocular muscle motility. Virtual surgical planning and 3-D printing can be used for large or complicated defects, especially those involving multiple orbital walls. Bone grafts or resorbable implants can be considered in younger patients (age < 6-11 years). Newer resorbable materials have improved safety profiles with less edema and foreign body reaction.
Indications for Resorbable Plating System Options Versus Traditional Non-resorbable Systems in the Pediatric Population
A major consideration is the growing facial skeleton so when non-resorbable plates are used, a second procedure is often recommended for removal to avoid bony overgrowth, plate migration, and potential growth disturbance. In the prepubescent patient, titanium plate removal may be performed three to six months after surgery.
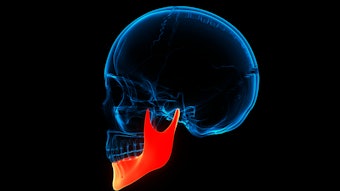
Fortunately, many pediatric fractures do not require operative intervention. Many mandible injuries are greenstick fractures and can be treated with a soft diet and observation. Minimally displaced fractures can be addressed with maxillomandibular fixation. In patients with developing dentition, this can include Erich arch bars, Risdon cables, custom acrylic splints, or skeletal suspension wires depending on the anatomy. Whereas significantly displaced, comminuted, or unsuccessfully reduced mandible fractures should be addressed with open reduction and internal fixation, typically at the inferior border to avoid tooth buds.
This topic was presented as Panel Presentation at the AAO-HNSF 2022 Annual Meeting & OTO Experience in Philadelphia, Pennsylvania. The panel was developed by the Facial Plastic and Reconstructive Surgery Education Committee (FPRSEC) and cosponsored by the Pediatric Otolaryngology Education Committee (POEC). Panelists were Lauren Bohm, MD, University of Michigan; Brianne Roby, MD, University of Minnesota; Jonathan Lee, MD, University of Massachusetts Baystate Health; and Nikita Gupta, MD, University of Kentucky.