The Diagnosis of Muscle Tension Dysphagia
MTDg is a diagnosis of exclusion that requires a comprehensive evaluation tailored to the patient being evaluated.
David G. Lott, MD, Christina H. Kang Rosow, MM, MS, CCC-SLP, James A. Curtis, PhD, CCC-SLP, Ashli O'Rourke, MD, and Gregory N. Postma, MD
Muscle Tension Dysphagia (MTDg) was originally described by Kang and colleagues in 2016.1 Like muscle tension dysphonia, MTDg is a condition whereby hyperactive and discoordinated muscle activity is hypothesized to be the underlying cause of a patient’s dysphagia. However, as with any new clinical entity, it is important to establish clearly defined diagnostic criteria. This is especially important given the sharp rise in clinical and research interests related to MTDg.2–7
Paramount to the practice of medicine is the tenant of “do no harm.” Inappropriate labeling of individuals with MTDg without proper evaluation can lead to a delay in the diagnosis of potentially life-threatening disease. Lack of clear diagnostic criteria can also negatively impact how research findings generalize across studies and to clinical practice. Therefore, there is a critical need to improve the transparency and standardization of the diagnosis of MTDg for both clinical and research purposes. It is our hope that this article will begin to address this gap by proposing a standardized framework used to carefully and comprehensively guide the diagnosis and management of MTDg in both clinical and research practices.
What is MTDg?
The symptom of dysphagia is typically caused by disordered sensory and/or motor function of the swallowing mechanism. Causes of dysphagia are thought to be multifactorial in nature, including changes in anatomy (e.g., tumor presence, postsurgical changes), connective tissue pliability (e.g., post-radiation therapy), afferent nerve function, somatosensory processing, motor control and coordination, motor nerve function, and peripheral muscle strength. MTDg suggests muscle tension of the pharynx and larynx is a significant factor contributing to the development of a patient’s dysphagia.
MTDg is currently believed to be a part of a spectrum of disorders known as laryngeal hypersensitivity/hyperresponsive disorders (LHS/LHR) (Figure 1). These disorders manifest as either sensory or motor abnormalities, or a combination of the two, and may impact any element of laryngeal function including breathing, voicing, and swallowing. Current research suggests that it is common for patients with LHS/LHR disorders to experience manifestation in more than one laryngeal function at any given time. One recent study by Kang and colleagues in 2021 reported that 65% of MTDg cases were associated with additional laryngeal hypersensitivity above and beyond MTDg.7
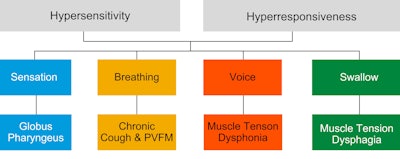 Figure 1. Laryngeal hypersensitivity/hyperresponsive disorders (LHS/LHR).
Figure 1. Laryngeal hypersensitivity/hyperresponsive disorders (LHS/LHR).
It is important to mention that MTDg may occur as a singular cause of a patient’s dysphagia, as a result of other disorders, or concurrently with other disorders. Therefore, clinicians should consider MTDg in addition to, or separate from, other potential dysphagia etiologies. The diagnostic evaluation, as discussed below, is meant to identify all possible etiologies for a patient’s dysphagia.
Diagnosis
MTDg is currently a diagnosis of exclusion. Because of this, a proper diagnosis of MTDg requires a thorough evaluation from skilled clinicians across multiple disciplines. Multidisciplinary input and collaboration are critical to the diagnosis of MTDg. The multidisciplinary team for the diagnosis of MTDg should include (at minimum) both an otolaryngologist with expertise evaluating oropharyngeal and esophageal anatomy and function and a speech-language pathologist with expertise in the evaluation, treatment, and management of dysphagia, laryngeal tension, and laryngeal hypersensitivity disorders. The role of both clinical professionals is to identify and/or rule out the presence of medical morbidities that may be leading to similar symptom profiles as MTDg and to identify the presence of hyperactive muscle tension as a probable cause of the dysphagia. The diagnostic framework for MTDg should include a minimum assessment of the following four domains:
- A comprehensive clinical swallow evaluation involving a thorough history and head and neck examination
- A laryngoscopic evaluation of the larynx and pharynx
- An instrumental evaluation of oropharyngeal swallowing
- An esophageal evaluation
Clinical Swallow Evaluation
The clinical swallow evaluation should include a thorough history and head and neck examination. The history should be symptom-driven with consideration to individual risk factors and identification of “red flag” signs or symptoms. This approach allows the clinician flexibility to tailor the evaluation process for each patient presentation. The clinical swallow evaluation serves two purposes. First, assessing voice use patterns (strain) during the patient interview and tension holding patterns during the head and neck examination assists in identifying muscle tension as a potential factor contributing to dysphagia. Second, identifying “red flag” signs or symptoms during the history and head and neck examination helps to rule out other medical morbidities.
The concept of “red flag” signs or symptoms is critical in the evaluation of a patient with suspected MTDg. This assists in identifying the presence of potentially life-threatening medical morbidities (e.g., esophageal cancer) or other conditions (e.g., reflux) that may be leading to a similar symptom profile. The default assessment of MTDg must be to suspect that any individual with presumed MTDg may have a much more serious underlying cause of their symptoms. A list of red flag signs or symptoms that should be reported in every clinical evaluation are outlined in Table 1.
Table 1. Red flag signs and/or symptoms of MTDg.
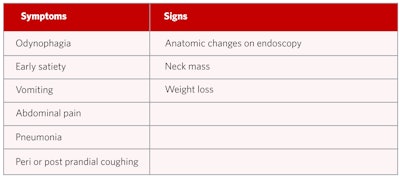
Although some of the signs and symptoms may be fairly obvious red flags, other less obvious ones need to be carefully elicited by the clinician to rule out potentially serious conditions unrelated to MTDg. One should also consider that the lack of symptom resolution with prescribed treatment is a relative red flag and should prompt the clinician to pursue further investigation. It cannot be stressed enough that a patient should not be diagnosed with MTDg until an appropriate evaluation has been completed.
Endoscopic Evaluation of the Pharynx and Larynx
A detailed endoscopic examination of the pharynx and larynx is the second necessary component of a comprehensive workup for MTDg. Like the clinical swallow evaluation, the endoscopic evaluation of the pharynx and larynx helps to identify muscle tension and rule out other medical morbidities. The endoscopic evaluation should be used to evaluate for mucosal lesions, anatomic defects, supraglottic hyperactivity, and (non-swallowing) function (e.g., vocal fold mobility, laryngeal diadochokinesis, pharyngeal squeeze maneuver, base of tongue retraction). Patients with concurrent voice changes, either from self-report or that was identified during the clinical swallow evaluation, should also have assessment of vocal fold vibration using videostroboscopy. Together, assessment of supraglottic activity and vocal fold vibration aid in identifying the presence of hyperactive muscle tension and discoordination, while assessment of anatomy and non-swallowing function assist in ruling out other issues.
Evaluation of Oropharyngeal Swallowing Function
Assessment of oropharyngeal swallowing is the third necessary component of a comprehensive assessment of MTDg. Examination of oropharyngeal swallowing function can be performed with either a modified barium swallow study (MBSS), also termed videofluoroscopic swallowing study (VFSS), or a flexible endoscopic evaluation of swallowing (FEES). The purpose of assessment of oropharyngeal swallow function using MBSS or FEES is to thoroughly evaluate the swallowing mechanism and anatomy. For this reason, while either FEES or MBSS would suffice, it is our belief that the MBSS is the superior examination in these patients as it allows for assessment of the pharyngoesophageal segment. Performance of the MBSS should be completed with a high frame rate (30 frames per second or continuous) as this allows for the detection of small hypopharyngeal and/or proximal esophageal webs. Additionally, since esophageal disorders may result in proximal dysphagia, at least an esophageal follow-through should be performed with the MBSS. Ideally, a dedicated esophagram would be performed, as discussed later.
Swallow function may appear “normal” on MBSS or FEES. In other words, traditional findings related to the presence of abnormal swallowing kinematics, pharyngeal residue, penetration, and aspiration may be absent. The absence of these findings does not preclude a diagnosis of MTDg since MTDg can include sensory or subtle functional changes not evaluated using FEES or MBSS. Furthermore, high resolution pharyngeal manometry (HRPM) may be used to supplement, but not replace, MBSS or FEES to assist with identifying hyperactive muscle activity during the swallow.
Evaluation of Esophageal Function
The purpose of evaluating esophageal function is to determine if the patient’s dysphagia is due to an esophageal cause. When and how to appropriately evaluate esophageal function in patients with suspected MTDg is perhaps the area of most controversy. The various methods that could be used to evaluate esophageal function for MTDg include barium esophagram, esophagoscopy, high resolution manometry, and/or pH-impedance testing. Selection of which method to use is tailored to the patient being evaluated. Sometimes a combination of these tests will be necessary to gain a full understanding of the potential sources of esophageal dysfunction causing the symptoms.
Barium esophagram or “barium swallow” is valuable for deriving anatomic information such as diverticuli, stricture, or the presence of a hiatal hernia. Visual examination by conventional sedated esophagoscopy or transnasal esophagoscopy has the benefit of being a diagnostic examination that gives detailed inspection of the mucosa but also can be therapeutic in that dilation can be completed as well. Additionally, biopsies may be obtained to rule out eosinophilic esophagitis or when lesions are noted. High-resolution manometry (HRM) with or without impedance is helpful in patients with suspected motility disorders and should be considered when radiographic or endoscopic testing are unrevealing but symptoms persist. Patients with suspected reflux may benefit from pH-impedance testing.
Conclusion
MTDg is a diagnosis of exclusion that requires a comprehensive evaluation tailored to the patient being evaluated. As such, we have proposed a framework that covers four necessary components. Within each component, the evaluation process should be individualized to the patient. It is clear that different patients may need to undergo different evaluation processes. However, each patient should be assessed broadly using the same four assessment domains. It is also reasonable that an individual who is suspected of having MTDg could begin a trial of therapy before the entire evaluation process is complete given pragmatic limitations. However, resolution of symptoms during the course of therapy in the presence of “red flags” during the clinical swallow evaluation should not negate the need to complete each of the four necessary components of the MTDg comprehensive workup.
References
- Kang CH, Hentz JG, Lott DG. Muscle Tension Dysphagia: Symptomology and theoretical framework. Otolaryngol Head Neck Surg. 2016;155(5):837-842. doi:10.1177/0194599816657013
- Yamazaki Y, Tohara H, Hara K, et al. Excessive anterior cervical muscle tone affects hyoid bone kinetics during swallowing in healthy individuals. Clin Interv Aging. 2017;120:1903-1910. doi:10.2147/CIA.S143175
- McGarey PO, Barone NA, Freeman M, Daniero JJ. Comorbid dysphagia and dyspnea in Muscle Tension Dysphonia: A global laryngeal musculoskeletal problem. OTO Open. 2018;2(3). doi:10.1177/2473974X18795671
- DePietro JD, Rubin S, Stein DJ, Golan H, Noordzij JP. Laryngeal manipulation for dysphagia with Muscle Tension Dysphonia. Dysphagia. 2018;33:468-473. doi:10.1007/s00455-018-9875-x
- Hamdan A-L, Khalifee E, Jaffal H, Ghanem A, El Hage A. Prevalence of dysphagia in patients with muscle tension dysphonia. J Laryngol Otol. April 2019:1-4. doi:10.1017/S0022215119000513
- Buckley DP, Vojtech JM, Stepp CE. Relative fundamental frequency in individuals with globus syndrome and Muscle Tension Dysphagia. J Voice. 2021. doi:10.1016/j.jvoice.2021.10.013
- Kang CH, Zhang N, Lott DG. Muscle Tension Dysphagia: Contributing factors and treatment efficacy. Ann Otol Rhinol Laryngol. 2021;130(7):674-681. doi:10.1177/0003489420966339