Shaping Meaningful Measures: A Patient-Centric Approach
The AAO-HNSF continues to move the needle for measures toward a patient-centric approach that spans the continuum of care.
Patient-Reported Outcomes Measures
CMS programs need to highly prioritize patient-reported outcome measures (PROMs) and measures using patient-generated data that represent critical information for shared decision-making and determining healthcare value. AAO-HNSF has continued to focus initiatives toward the Meaningful Measures framework during the past year, including progress toward refinements to the age-related hearing loss (ARHL) PROs survey in Reg-entSM with continued piloting with several Reg-ent practices. In addition, programming within Reg-ent of the next PROM Sino-Nasal Outcome Test (SNOT-22), has begun.
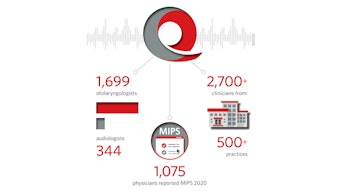
MIPS Value Pathways
As CMS continues to design, evaluate, and implement the MVP program, it requested to hear from stakeholders and receive their feedback on policies under consideration for future implementation. CMS has identified its transition from traditional Merit-based Incentive Payment System (MIPS) to MVP as an additional way to reduce burden to physicians, e.g., transitioning from reporting on multiple measures, which may or may not be reflective of practice, to one set of disease-specific measurements and quality improvement efforts, which can demonstrate the high-quality care that is provided to patients.
In January, the AAO-HNS submitted a comment letter supportive of the concept of MVPs, as it is likely the only pathway allowing most specialty physicians, such as otolaryngologists, to be able to participate in Advanced Payment Models (APMs). In our comments, we urged CMS to consider comments regarding the MVP program’s purpose, design, implementation, and scores.
The AAO-HNS stands ready to work with CMS to ensure that the new pathway, if implemented, improves value, reduces burden, and better informs patient choice. In anticipation of the CMS transition from the current MIPS model toward MVP, AAO-HNS submitted three MVP candidates—on Hearing Loss, Early Oral Cavity Cancer, and Allergic Rhinitis—to CMS for comments in February. AAO-HNS had also submitted input to CMS on episode-based cost measure development. In addition, the AAO-HNS is integrating a more rigorous measure testing process for Qualified Clinical Data Registry (QCDR) measures in Reg-ent and will begin working on this to ensure face validity and to eventually incorporate full measure testing for Reg-ent measures. QCDR measures must be fully tested at the clinician level in order to be considered for inclusion in MVPs.
Quality Measures Publications
For 2021, three publications in Otolaryngology–Head and Neck Surgery highlight the continued efforts of the AAO-HNSF to develop quality measures that are relevant to otolaryngologists.
Executive Summary: “Evidence-Based Performance Measures for Rhinoplasty: A Multidisciplinary Performance Measure Set” was published in February. This article provides an overview of the Rhinoplasty Performance Measurement Workgroup, a multidisciplinary collaboration of the AAO-HNSF with the American Society of Plastic Surgeons, and the American Academy of Facial Plastic and Reconstructive Surgery. The workgroup developed the rhinoplasty quality measure set within the framework of the 2018 AAO-HNSF Clinical Practice Guideline: Improving Nasal Form and Function after Rhinoplasty and ultimately identified one outcome measure and three process measures.
“Quality Improvement in Otolaryngology–Head and Neck Surgery: Age-Related Hearing Loss Measures,” published in March, discusses the process by which the expert-comprised Measure Development Group reached consensus on four de novo measures listed below. These measures were created for the diagnosis and treatment of ARHL disorders, including bilateral presbycusis and symmetric sensorineural hearing loss, and they are intended to assist providers in enhancing quality of care.
- Screening for Hearing Loss in Older Adults
- Audiometric Evaluation for Older Adults with Hearing Loss
- Advanced Diagnostic Imaging for ARHL—Avoidance of Inappropriate Use
- Shared Decision-Making for Treatment Options for ARHL
“Quality Improvement in Otolaryngology–Head and Neck Surgery: Developing Registry-Enabled Quality Measures from Guidelines for Cerumen Impaction and Allergic Rhinitis Using a Transparent and Systematic Process,” which published in May 2021, provides an overview of the process to support systematic translation of clinical practice guidelines (CPGs) into electronic quality measures using a transparent and reproducible pathway by ECRI (formerly the Emergency Care Research Institute). This process was piloted with the AAO-HNSF to create electronic quality measures based on two AAO-HNSF CPGs.
Several of the quality measures developed from these processes were approved by CMS for use in the Reg-ent registry. These measures publications can be accessed at https://www.entnet.org/quality-practice/quality-measurement/aao-hnsf-measure-publications/.










![05 Hpv Vaccination [converted]](https://img.ascendmedia.com/files/base/ascend/hh/image/2021/06/05_HPV_Vaccination__Converted_.60d0a1f25afe4.png?auto=format%2Ccompress&fit=crop&h=191&q=70&rect=45%2C0%2C1830%2C1830&w=340)