Out of Committee: OREBM and PSQI | Research and Quality Supported through Committee Work
These efforts contribute to the success of the AAO-HNS/F mission by helping members to achieve excellence and provide the best possible care to patients. The COVID-19 pandemic underscored the importance of the committee structure.
Outcomes Research and Evidence-Based Medicine
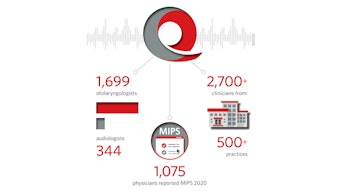
Research and Quality staff support the work of the Outcomes Research and Evidence-Based Medicine (OREBM) and the Patient Safety Quality Improvement (PSQI) Committees, which continue to add to their highly productive work history of contributing research, publications, and Annual Meeting panel presentations designed to assist members in all areas of practice.
The OREBM Committee, under the leadership of Chair Michael J. Brenner, MD, continues to provide expertise in the areas of health services research and evidence-based medicine, including outcomes and comparative-effectiveness research generally and specifically in otolaryngology-head and neck surgery. OREBM has furthered its charge relating to improving the evidence base in 2020-2021 by spearheading several innovative collaborative endeavors spanning across committees and Academy goals. These efforts have addressed the core mission of the AAO-HNS/F by providing tools, conducting outcomes research, and enhancing the evidence-based medicine capabilities of the Academy.
Most notably, the OREBM Committee continues to contribute to 2021 activities, which include publication spotlights for inclusion in the AAO-HNS Bulletin. Article reviews include topics on steroid-eluting sinus stents and growing the evidence base for healthcare disparities and social determinants of health research. These articles highlight current publications with significant findings for clinical or surgical practice in otolaryngology-head and neck surgery. The OREBM Committee actively submitted 22 abstracts and proposals in preparation for the AAO-HNSF 2021 Annual Meeting & OTO Experience in Los Angeles, California.
The OREBM committee has drawn on reserves of energy and talent among its members to advance the art, science, and ethical practice of otolaryngology-head and neck surgery through education, research, and lifelong learning.
Patient Safety and Quality Improvement
The Patient Safety and Quality Improvement (PSQI) Committee, under the leadership of the Co-Chairs C.W. David Chang, MD, and Emily F. Boss, MD, MPH, and Chair-Elect Soham Roy, MD, continues to raise awareness within the Academy of patient safety and quality improvement issues. The committee educates members about evidence-based guidelines, practice standards, and other systems that enhance quality of care. In addition, the committee identifies products, tools, services, and processes that lead to safer care of otolaryngology-head and neck surgery patients and assists the Academy in making them known and available to its membership. PSQI actively coordinates with other committees of the Academy and the Foundation and with members of other relevant specialty societies on issues pertaining to patient safety and quality improvement. The committee provides input to prioritize the development of guidelines and performance measures used to assess and improve the quality of care for otolaryngology-head and neck surgery patients. The committee is also responsible for the review, validation, and approval of requests to survey the AAO-HNS membership on topics related to patient safety and quality improvement, as assigned.
To highlight this past year for the PSQI Committee and in response to the rapid need for COVID-19 information, the AAO-HNS created a COVID-19 podcast series, with the first episode titled “Patient Safety.” Quickly, symptoms of olfactory and gustatory dysfunction (OGD) were noted to be common findings suspicious of COVID-19 diagnosis. As charged by James C. Denneny III, MD, AAO-HNS/F Executive Vice President and CEO, a pre-existing AAO-HNS patient-safety reporting tool was restructured to crowd source OGD symptoms in relationship to timing and risk factors of COVID-19 as self-reported by physicians and patients from around the world. Such research contributed to the addition of anosmia as a potential cardinal symptom of COVID-19 by the Centers for Disease Control and Prevention.1 In preparation for the AAO-HNSF 2021 Annual Meeting & OTO Experience in Los Angeles, California, the PSQI Committee also submitted 19 abstract proposals.
The direction of both committees was significantly influenced by the emergence of the COVID-19 pandemic, which required unprecedented levels of cooperation across the committee structure of the Academy to author several COVID-related manuscripts on safety recommendations after tracheostomy,2 tracheostomy protocols,3 safe airway management,4 difficult airway management and aerosol-generating procedures, and healthcare disparities in head and neck cancer,5 as well as other high priority areas for the specialty. The AAO-HNS Statement on Treatment of Idiopathic Facial Paralysis (Bell’s Palsy) During the COVID-19 Pandemic was created in collaboration with multiple committee stakeholders (PSQI, OREBM, Infectious Disease, Otology and Neurotology Education, Plastic and Reconstructive Surgery, Facial Plastic and Reconstructive Education) and in consultation with infectious disease physicians. Continued strong relations between the PSQI and OREBM Committees have produced publications coauthored by members from both committees. In addition to the above, other articles include evaluating intraoperative sentinel events,6 oral intubation attempts in patients with laryngectomy,7 and foreign body aspiration in children.8 With members of the Pediatric Otolaryngology Education Committee, a literature review was conducted and guidance on pediatric tracheostomy care was published.
These efforts contribute to the success of the AAO-HNS/F mission by helping members to achieve excellence and provide the best possible care to patients. The COVID-19 pandemic underscored the importance of the committee structure in meeting significant needs for patient and provider guidance pertaining to otolaryngology.
References
1. Kaye R, Chang CWD, Kazahaya K, Brereton J, Denneny JC. COVID-19 anosmia reporting tool: initial findings. Otolaryngol Head Neck Surg. 2020;163(1):132-134. doi:10.1177/0194599820922992
2. Meister KD, Pandian V, Hillel AT, et al. Multidisciplinary safety recommendations after tracheostomy during COVID-19 pandemic: state of the art review. Otolaryngol Head Neck Surg. 2021;164(5):984-1000. doi: 10.1177/0194599820961990.
3. Bier-Laning C, Cramer JD, Roy S, et al. Tracheostomy during the COVID-19 pandemic: comparison of international perioperative care protocols and practices in 26 countries. Otolaryngol Head Neck Surg. Published online November 3, 2020. doi: 10.1177/0194599820961985.
4. Balakrishnan K, Schechtman S, Hogikyan ND, Teoh AYB, McGrath B, Brenner MJ. COVID-19 pandemic: what every otolaryngologist-head and neck surgeon needs to know for safe airway management. Otolaryngol Head Neck Surg. 2020;162(6):804-808. doi: 10.1177/0194599820919751.
5. Graboyes E, Cramer J, Balakrishnan K, et al. COVID-19 pandemic and health care disparities in head and neck cancer: scanning the horizon. Head Neck. 2020;42(7):1555-1559. doi: 10.1002/hed.26345.
6. Cramer JD, Balakrishnan K, Roy S, et al. Intraoperative sentinel events in the era of surgical safety checklists: results of a national survey. OTO Open. 2020;4(4):2473974X20975731. doi: 10.1177/2473974X20975731.
7. Brenner MJ, Cramer JD, McGrath BA, et al. Oral intubation attempts in patients with a laryngectomy: a significant safety threat. Otolaryngol Head Neck Surg. 2021;164(5):1040-1043. doi: 10.1177/0194599820960728.
8. Cramer JD, Meraj T, Lavin JM, Boss EF. Object-related aspiration deaths in children and adolescents in the United States, 1968 to 2017. JAMA. 2019;322(20):2020-2022. doi: 10.1001/jama.2019.15375.








![05 Hpv Vaccination [converted]](https://img.ascendmedia.com/files/base/ascend/hh/image/2021/06/05_HPV_Vaccination__Converted_.60d0a1f25afe4.png?auto=format%2Ccompress&fit=crop&h=191&q=70&rect=45%2C0%2C1830%2C1830&w=340)