Quality…You Can Make a Difference
As new measures of medicine rapidly evolve and engulf us, Research and Quality Improvement reign high as parameters that shape and define our practices. We must incorporate new knowledge into our patient care, and remain vigilant about external expectations and grading schemes. The word “Quality” is tossed around frequently and freely in the medical arena. The stakes of adequate, or preferably, superior quality continue to rise with reimbursement and recognition tied into this precious seven letter word. And yet, what is quality? We all have a gestalt “feeling” about high quality service and products, yet defining the term proves to be a bit nebulous. Webster defines quality as “a high level of value or excellence.” Physician quality assessments are running amok with valuations based on price (regardless of disease severity), results (which may not be equally comparable), compliance (with rules imposed by non-medical entities), and even waiting room decor. Physicians recognize that high quality relates to developing and nurturing effective interpersonal relationships with our patients, creating successful outcomes based on our interventions and treatments, and maintaining our patients’ health through lifestyle modifications and early recognition of significant symptoms. Yet the quality measures upon which we are judged revolve around different parameters—meaningful use adherence in our EHR systems, PQRS reporting, and cost and utilization reduction. Important? Perhaps. But directly related to our effectiveness and quality as healthcare providers? Not yet. Physicians must help define the measures by which we are judged. We are fortunate that able otolaryngologists across the nation have taken significant leadership roles in areas such as Clinical Practice Guidelines, and new appropriate PQRS measures. By engaging in the rule making process, we influence our own future directions and constraints. At the grassroots level, the BOG Socioeconomic and Grassroots (SEGR) Committee is tackling many of these quality related issues, and encourages all otolaryngologists to share their concerns about how we can improve the healthcare landscape that has been thrust upon us. The Regionalization Plan, dividing the country into 10 geographic regions—each with a regional representative leader serves to coordinate regional issues and becomes an avenue to interconnect all 50 states in an efficient and fluid fashion. By listening and learning from each other, we gain collective wisdom and strategies. The SEGR national polls during the past two years have provided excellent input into two hot issues—pediatric subcertification and clinical practice guidelines. Through these polls, membership has contributed valuable thoughts about how we can improve our care and our quality. Each annual poll will continue to address pertinent issues. Please take the time to complete and return these polls, we want to hear your voice. Physician grading based on quality and cost is not disappearing. It is incumbent on each and every otolaryngologist, from resident to young physician to seasoned practitioners, to participate in the discussions and the polls. Contact your regional rep with any local issues. Use ENTConnect, which now has pages devoted to each separate region. By taking the difficult steps in taking charge and responsibility for our own measures, we can help shape the playing field for ourselves, our patients, and our future. * Stay alert and connect: bog@entnet.org
 Ken Yanagisawa, MD, Vice Chair, BOG SEGR Committee
Ken Yanagisawa, MD, Vice Chair, BOG SEGR CommitteeAs new measures of medicine rapidly evolve and engulf us, Research and Quality Improvement reign high as parameters that shape and define our practices. We must incorporate new knowledge into our patient care, and remain vigilant about external expectations and grading schemes. The word “Quality” is tossed around frequently and freely in the medical arena. The stakes of adequate, or preferably, superior quality continue to rise with reimbursement and recognition tied into this precious seven letter word. And yet, what is quality? We all have a gestalt “feeling” about high quality service and products, yet defining the term proves to be a bit nebulous.
Webster defines quality as “a high level of value or excellence.”
Physician quality assessments are running amok with valuations based on price (regardless of disease severity), results (which may not be equally comparable), compliance (with rules imposed by non-medical entities), and even waiting room decor.
Physicians recognize that high quality relates to developing and nurturing effective interpersonal relationships with our patients, creating successful outcomes based on our interventions and treatments, and maintaining our patients’ health through lifestyle modifications and early recognition of significant symptoms. Yet the quality measures upon which we are judged revolve around different parameters—meaningful use adherence in our EHR systems, PQRS reporting, and cost and utilization reduction. Important? Perhaps. But directly related to our effectiveness and quality as healthcare providers? Not yet.
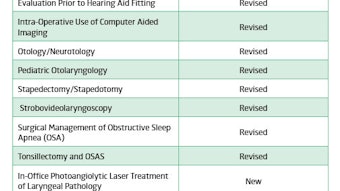
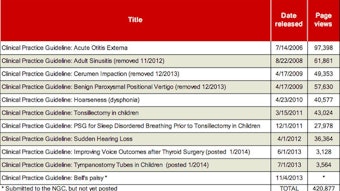
Physicians must help define the measures by which we are judged. We are fortunate that able otolaryngologists across the nation have taken significant leadership roles in areas such as Clinical Practice Guidelines, and new appropriate PQRS measures. By engaging in the rule making process, we influence our own future directions and constraints.
At the grassroots level, the BOG Socioeconomic and Grassroots (SEGR) Committee is tackling many of these quality related issues, and encourages all otolaryngologists to share their concerns about how we can improve the healthcare landscape that has been thrust upon us.
The Regionalization Plan, dividing the country into 10 geographic regions—each with a regional representative leader serves to coordinate regional issues and becomes an avenue to interconnect all 50 states in an efficient and fluid fashion. By listening and learning from each other, we gain collective wisdom and strategies.
The SEGR national polls during the past two years have provided excellent input into two hot issues—pediatric subcertification and clinical practice guidelines. Through these polls, membership has contributed valuable thoughts about how we can improve our care and our quality. Each annual poll will continue to address pertinent issues. Please take the time to complete and return these polls, we want to hear your voice.
Physician grading based on quality and cost is not disappearing. It is incumbent on each and every otolaryngologist, from resident to young physician to seasoned practitioners, to participate in the discussions and the polls. Contact your regional rep with any local issues. Use ENTConnect, which now has pages devoted to each separate region. By taking the difficult steps in taking charge and responsibility for our own measures, we can help shape the playing field for ourselves, our patients, and our future.
* Stay alert and connect: bog@entnet.org