2014 Hospital Outpatient Prospective Payment and Ambulatory Surgical Center Payment Systems Proposed Rule
On July 8, the Centers for Medicare & Medicaid Services (CMS) released its 2014 proposed rule for the hospital outpatient prospective payment (OPPS) and ambulatory surgical center (ASC) payment systems. Below are a few important changes relevant to otolaryngology for CY 2014. A complete summary of the proposed rule can be found at http://www.entnet.org/Practice/CMS-News.cfm. Hospital Outpatient Prospective Payment System (OPPS) As members know, OPPS payments cover facility resources including equipment, supplies, and hospital staff, but do not pay for the services of physicians and non-physician practitioners who are paid separately under the Medicare Physician Fee Schedule (MPFS). All services under the OPPS are technical and are classified into groups called Ambulatory Payment Classifications (APCs). Services in each APC are grouped by clinically similar services that require the use of similar resources. A payment rate is established for each APC using two-year-old hospital claims data adjusted by individual hospitals cost-to-charge ratios. The APC national payment rates are adjusted for geographic cost differences, and payment rates and policies are updated annually through rulemaking. OPPS 2014 Proposed Payment Rates For CY 2014, CMS proposes a hospital outpatient department conversion factor rate increase of 1.8 percent. CMS has also proposed to continue the statutory -2 percent reduction in payments for hospitals that fail to meet the hospital outpatient quality reporting (OQR) requirements. See the summary link from paragraph one to access changes in reimbursement under the proposed rule for CY 2014 for the 100 most frequently billed ENT services in the OPPS setting. Updates Affecting OPPS Payments In CY 2014, CMS has proposed to continue the changes made in 2013 to base the relative weights on geometric mean costs rather than previously utilized median costs. It will continue to use these weights to set a cost-to-charge ratio within an APC to determine payment for services within an APC. In CY 2014, CMS proposes several significant changes to their methodology to calculate APC payments, including: Establishing comprehensive APCs for 38 device-dependent services and applying a single payment for the comprehensive service based on all OPPS payable charges on the claim Expanding the types of services that are packaged and not paid separately Replacing the current five levels of visit codes for the clinic with three new Level II HCPCS codes, which represent a single level of payment for each of the three visit types Changes to otolaryngology related to many of these policies are outlined below, however, members seeking additional information can access our full summary via the link above, which includes a complete list of APCs and changes to their payment rates. New Comprehensive APCs In an effort to improve accuracy and transparency of certain device-dependent procedures, CMS proposes 29 new comprehensive APCs to prospectively pay for the most costly device-dependent services. These APCs will replace 29 of the most costly device-dependent APCs. A comprehensive APC would be defined to include the provision of a primary service and all adjunctive services provided to support the delivery of the primary service. Under the proposal, the entire claim, including the primary service, would be associated with a single comprehensive service and all costs reported on the claim would be assigned to that service. The comprehensive APC would treat all individually reported codes as representing components of the comprehensive service and would make a single payment based on the cost of all individually reported codes, representing provision of the primary service, and all adjunctive services provided to support delivery of the primary service. CMS believes this will increase the accuracy of the payment for the comprehensive service and also increase the stability of the payment from year to year. CMS proposes to include packaged services and supplies; adjunctive services; devices, durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS); OPD services reported by therapy codes that are provided within the perioperative period of the primary service; hospital room and board revue centers; and hospital-administered drugs as part of these new comprehensive APCs. Payment for comprehensive APCs would be made for the largest comprehensive payment associated with the claim based on the listed CPT codes, however, all costs on the claim will be considered in ratesetting for the comprehensive APC. Of note, APC 0259, which includes CPT 69930 Implant Cochlear Device will be included as a comprehensive APC for CY 2014. Proposed New Packaging Policies for CY 2014 For CY 2014, CMS proposes to add the following five items and services to those that will be packaged under the OPPS. Drugs, biologicals, and radiopharmaceuticals that function as supplies when used in a diagnostic test or procedure Drugs and biologicals that function as supplies or devices when used in a surgical procedure Clinical diagnostic laboratory tests Procedures described by add-on codes Ancillary services (status indicator “X”) The packaging policies that influence otolaryngology are discussed in greater detail in our full summary; however, we note that items 2-5 on the list above capture at least one ENT service. Affected services include laryngology procedures, head and neck imaging services, audiology, and SLP services. Access the online summary for a full list of affected CPT codes and APCs by policy proposal. CMS also indicates it is considering a proposal for 2015 that would conditionally package all imaging services with any associated surgical procedures. Imaging services not provided with a surgical procedure would continue to either be separately paid according to a standard clinical APC or a composite APC. OPPS Payment for Hospital Outpatient Visits For CY 2014, CMS is proposing to replace the current five levels of visit codes describing clinic visits, Type A and Type B emergency department visits, and critical care services with three alphanumeric Level II HCPCS codes representing a single level of payment for three types of visits. CMS believes a policy that recognizes a single visit level for clinic visits, Type A ED visits, and Type B ED visits for payment under the OPPS is appropriate for several reasons, including: To incentivize hospitals to maximize efficiency Remove incentives of providing unnecessary services or expending unnecessary resources Reduce administrative burden Eliminate the need to distinguish between new and established patients Eliminate incentives to “upcode” patients whose visits don’t fall into a clear category Under this proposal, beginning in 2014, physicians and hospitals would begin using the coding structure displayed in the chart to report their visits in the OPPS setting. Supervision of Outpatient Therapeutic Services in CAHs and Small Rural Hospitals CMS proposed to end its non-enforcement policy requiring direct supervision of outpatient therapeutic services in CAHs and small rural hospitals. Thus, for years beginning with 2014, CAHs and small rural hospitals would have to comply with the CMS supervision policy, which requires direct supervision of therapeutic services except for those that CMS identifies as appropriate for general supervision, based on input from the Advisory Panel on Hospital Outpatient Payment (Advisory Panel). CMS believes it is appropriate to let this grace period expire to ensure the quality and safety of hospital and CAH outpatient therapeutic services provided by Medicare. Supervision for Observation Services CMS also clarified that for observation services, if the supervising physician or appropriate non-physician practitioner determines and documents in the medical record that the beneficiary is stable and may be transitioned to general supervision, general supervision may be furnished for the duration of the service. Medicare will not require an additional initiation period(s) of direct supervision during the service. CMS believes this clarification will assist hospitals in furnishing the required supervision of observation services without undue burden on their staff. Hospital Outpatient Quality Reporting (OQR) Program As established in previous rules, hospitals will continue to face a -2 percent reduction to their OPD fee schedule payments for failure to report on quality measures in the OQR Program in CY 2014. Program measures and details on timing and reporting periods can be accessed on the CMS Quality Net website at https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier2&cid=1191255879384. For 2014 reporting, CMS proposes five new quality measures and removes two measures from the OQR program for CY 2016 payment. None of the five new measures are applicable to our specialty; however, one of the two measures proposed for deletion (Transition Record with Specified Elements Received by Discharged Patients) may have been reportable by ENTs. Ambulatory Surgical Centers CMS performs an annual review of the legislative history and regulatory policies regarding changes to the lists of codes and payment rates for covered surgical procedures and covered ancillary services in an Ambulatory Surgical Center (ASC) setting. Covered surgical procedures in the ASC setting are defined as procedures that would not be expected to pose a significant risk to the beneficiary’s safety when performed in an ASC and that would not be expected to require active medical monitoring and care at midnight following the procedure. ASC 2014 Proposed Payment Rates For CY 2014, CMS proposes a .9 percent increase to the ASC conversion factor. The table above reflects the major categories of procedures in the ASC setting, the amount paid to each of those settings in 2013, and the estimated percentage change in payments to those categories for 2014. Of note, otolaryngology procedures fall within several of the key categories, including Eye, Integumentary, Auditory, Lymphatic, etc. Ambulatory Surgical Center Quality Reporting Program (ASCQR) In 2012, CMS finalized the implementation of an ASC quality reporting program (ASCQR), which will begin with 2014 payment determination. Quality measures have been adopted for the calendar years 2014-2016. The measures can be found on the CMS Quality Net website previously referenced. CMS continues their proposal to apply a -2 percent payment reduction for ASCs that fail to properly report their quality data in CY 2014. Penalties will be applied in CY 2016 payments based on 2014 reporting.
On July 8, the Centers for Medicare & Medicaid Services (CMS) released its 2014 proposed rule for the hospital outpatient prospective payment (OPPS) and ambulatory surgical center (ASC) payment systems. Below are a few important changes relevant to otolaryngology for CY 2014. A complete summary of the proposed rule can be found at http://www.entnet.org/Practice/CMS-News.cfm.
Hospital Outpatient Prospective Payment System (OPPS)
As members know, OPPS payments cover facility resources including equipment, supplies, and hospital staff, but do not pay for the services of physicians and non-physician practitioners who are paid separately under the Medicare Physician Fee Schedule (MPFS). All services under the OPPS are technical and are classified into groups called Ambulatory Payment Classifications (APCs). Services in each APC are grouped by clinically similar services that require the use of similar resources. A payment rate is established for each APC using two-year-old hospital claims data adjusted by individual hospitals cost-to-charge ratios. The APC national payment rates are adjusted for geographic cost differences, and payment rates and policies are updated annually through rulemaking.
OPPS 2014 Proposed Payment Rates
For CY 2014, CMS proposes a hospital outpatient department conversion factor rate increase of 1.8 percent. CMS has also proposed to continue the statutory -2 percent reduction in payments for hospitals that fail to meet the hospital outpatient quality reporting (OQR) requirements. See the summary link from paragraph one to access changes in reimbursement under the proposed rule for CY 2014 for the 100 most frequently billed ENT services in the OPPS setting.

In CY 2014, CMS has proposed to continue the changes made in 2013 to base the relative weights on geometric mean costs rather than previously utilized median costs. It will continue to use these weights to set a cost-to-charge ratio within an APC to determine payment for services within an APC. In CY 2014, CMS proposes several significant changes to their methodology to calculate APC payments, including:
- Establishing comprehensive APCs for 38 device-dependent services and applying a single payment for the comprehensive service based on all OPPS payable charges on the claim
- Expanding the types of services that are packaged and not paid separately
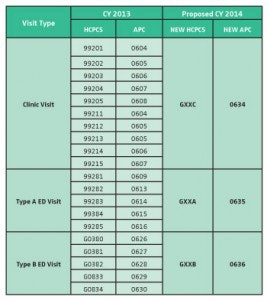
- Replacing the current five levels of visit codes for the clinic with three new Level II HCPCS codes, which represent a single level of payment for each of the three visit types
Changes to otolaryngology related to many of these policies are outlined below, however, members seeking additional information can access our full summary via the link above, which includes a complete list of APCs and changes to their payment rates.
New Comprehensive APCs
In an effort to improve accuracy and transparency of certain device-dependent procedures, CMS proposes 29 new comprehensive APCs to prospectively pay for the most costly device-dependent services.
These APCs will replace 29 of the most costly device-dependent APCs. A comprehensive APC would be defined to include the provision of a primary service and all adjunctive services provided to support the delivery of the primary service. Under the proposal, the entire claim, including the primary service, would be associated with a single comprehensive service and all costs reported on the claim would be assigned to that service.
The comprehensive APC would treat all individually reported codes as representing components of the comprehensive service and would make a single payment based on the cost of all individually reported codes, representing provision of the primary service, and all adjunctive services provided to support delivery of the primary service. CMS believes this will increase the accuracy of the payment for the comprehensive service and also increase the stability of the payment from year to year.
Proposed New Packaging Policies for CY 2014
For CY 2014, CMS proposes to add the following five items and services to those that will be packaged under the OPPS.
- Drugs, biologicals, and radiopharmaceuticals that function as supplies when used in a diagnostic test or procedure
- Drugs and biologicals that function as supplies or devices when used in a surgical procedure
- Clinical diagnostic laboratory tests
- Procedures described by add-on codes
- Ancillary services (status indicator “X”)
The packaging policies that influence otolaryngology are discussed in greater detail in our full summary; however, we note that items 2-5 on the list above capture at least one ENT service. Affected services include laryngology procedures, head and neck imaging services, audiology, and SLP services. Access the online summary for a full list of affected CPT codes and APCs by policy proposal.
CMS also indicates it is considering a proposal for 2015 that would conditionally package all imaging services with any associated surgical procedures. Imaging services not provided with a surgical procedure would continue to either be separately paid according to a standard clinical APC or a composite APC.
OPPS Payment for Hospital Outpatient Visits
For CY 2014, CMS is proposing to replace the current five levels of visit codes describing clinic visits, Type A and Type B emergency department visits, and critical care services with three alphanumeric Level II HCPCS codes representing a single level of payment for three types of visits. CMS believes a policy that recognizes a single visit level for clinic visits, Type A ED visits, and Type B ED visits for payment under the OPPS is appropriate for several reasons, including:
- To incentivize hospitals to maximize efficiency
- Remove incentives of providing unnecessary services or expending unnecessary resources
- Reduce administrative burden
- Eliminate the need to distinguish between new and established patients
- Eliminate incentives to “upcode” patients whose visits don’t fall into a clear category
Under this proposal, beginning in 2014, physicians and hospitals would begin using the coding structure displayed in the chart to report their visits in the OPPS setting.
CMS proposed to end its non-enforcement policy requiring direct supervision of outpatient therapeutic services in CAHs and small rural hospitals. Thus, for years beginning with 2014, CAHs and small rural hospitals would have to comply with the CMS supervision policy, which requires direct supervision of therapeutic services except for those that CMS identifies as appropriate for general supervision, based on input from the Advisory Panel on Hospital Outpatient Payment (Advisory Panel). CMS believes it is appropriate to let this grace period expire to ensure the quality and safety of hospital and CAH outpatient therapeutic services provided by Medicare.
Supervision for Observation Services
CMS also clarified that for observation services, if the supervising physician or appropriate non-physician practitioner determines and documents in the medical record that the beneficiary is stable and may be transitioned to general supervision, general supervision may be furnished for the duration of the service. Medicare will not require an additional initiation period(s) of direct supervision during the service. CMS believes this clarification will assist hospitals in furnishing the required supervision of observation services without undue burden on their staff.
Hospital Outpatient Quality Reporting (OQR) Program
As established in previous rules, hospitals will continue to face a -2 percent reduction to their OPD fee schedule payments for failure to report on quality measures in the OQR Program in CY 2014. Program measures and details on timing and reporting periods can be accessed on the CMS Quality Net website at https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier2&cid=1191255879384.
For 2014 reporting, CMS proposes five new quality measures and removes two measures from the OQR program for CY 2016 payment. None of the five new measures are applicable to our specialty; however, one of the two measures proposed for deletion (Transition Record with Specified Elements Received by Discharged Patients) may have been reportable by ENTs.
Ambulatory Surgical Centers
CMS performs an annual review of the legislative history and regulatory policies regarding changes to the lists of codes and payment rates for covered surgical procedures and covered ancillary services in an Ambulatory Surgical Center (ASC) setting. Covered surgical procedures in the ASC setting are defined as procedures that would not be expected to pose a significant risk to the beneficiary’s safety when performed in an ASC and that would not be expected to require active medical monitoring and care at midnight following the procedure.
ASC 2014 Proposed Payment Rates
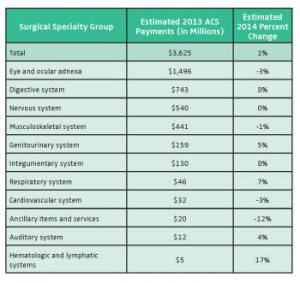
For CY 2014, CMS proposes a .9 percent increase to the ASC conversion factor. The table above reflects the major categories of procedures in the ASC setting, the amount paid to each of those settings in 2013, and the estimated percentage change in payments to those categories for 2014. Of note, otolaryngology procedures fall within several of the key categories, including Eye, Integumentary, Auditory, Lymphatic, etc.
Ambulatory Surgical Center Quality Reporting Program (ASCQR)
In 2012, CMS finalized the implementation of an ASC quality reporting program (ASCQR), which will begin with 2014 payment determination. Quality measures have been adopted for the calendar years 2014-2016. The measures can be found on the CMS Quality Net website previously referenced.
CMS continues their proposal to apply a -2 percent payment reduction for ASCs that fail to properly report their quality data in CY 2014. Penalties will be applied in CY 2016 payments based on 2014 reporting.