Committing to Self-government
Each October signals the tenure of a new round of Academy leadership. Not only do we inaugurate and honor a new Academy president, but a significant number of board members of both the Academy and the Foundation, as well as committee members and chairs, turn over each year. As I reflect on the “changing of the guard,” I experience two strong emotional responses. First, I am continually amazed and honored to be allowed to work so closely with such effective, selfless, and dedicated leadership. Working so closely with these remarkable men and women inspires me with confidence for the future. It is reassuring to know that we have an endless supply of talent and inspirational leadership. Second, my gratitude for the voluntary service represented by these leaders (emblematic of the culture of service that pervades our entire membership) is hard to put into words. So it is with great thanks and some sadness that we say “thank you” to James L. Netterville, MD, for his very personable, gracious, and effective leadership during the last year, and welcome with enthusiasm and anticipation the energy and guidance of our new president, Richard W. Waguespack, MD. As you all know, for nearly two decades we have alternated the selection of many of our officers, board, and committees members between community-based and academic otolaryngologists. In that manner, directly elected board directors, Nominating Committee members, as well as the president always bring the perspective of our entire membership, not just a popular or more vocal segment, to the table. This is a timely reminder, since this October issue of the Bulletin devotes focus to our membership and several committees. The structure of our Boards of Directors, the BOG, and our relationship with state, regional, or other specialty societies is designed to strike the optimal balance between the common ground that unites all of us as otolaryngologists and the desired autonomy of smaller societies who effectively provide community, subspecialty, or other interest or focus. The manner in which humans organize themselves to achieve things together that they could not achieve alone makes for interesting study. Whether forming a new neighborhood tree house club or a new nation, humans have sought safety, camaraderie, solace, community, or collective action with likeminded people since before recorded history. While the consequences of the boundaries we formally place around our relationships, and the number of “groups” we feel a kinship with has a serious impact on many aspects of our lives, some of what we learn over time makes us ask, “What were they thinking?” (Or, perhaps more to the point, “What were we thinking?!”) In his book, How the States Got Their Shapes, Mark Stein comments on the tremendous insight to be gained from researching this question. “Far more knowledge results from exploring why a set of conditions exists than from simply accepting those conditions and committing them to memory. Asking why a state has the borders it does unlocks a history of human struggles–far more history…” than the question implies. In studying why our geographic boundaries are the way they are, we learn about politics, war, grants, gifts, generosity, forgiveness, complaisance, incompetence, resignation, and regret. We discover the challenge of overcoming the inertia of culture, the bonds of familiarity, and the fear of the uncertain. These ideas are affecting how we move forward as otolaryngologists in both our internal and external environments. Internally, we have for years benefited from addressing the challenge of asking why we are organized the way we are, why we do things the way we do, and are our traditions, assumptions, and expectations still valid and relevant. We are drafting an entirely new version of our Member Handbook, complete with standard operating procedures, documentation of processes, and accurate and updated application of bylaws, policies, and positions that benefit our members, and by extension, our patients. Externally, we are being forced by economics, politics, and our professional desire to be the best to challenge foundational assumptions of how we organize healthcare, delivery and payment models, and methods for ensuring the highest quality of care can be delivered with the most effective utilization of resources. As we return to our practices after another successful Annual Meeting & OTO EXPOSM, let us meet the challenge to bring out the best in each other, professionally, personally, and organizationally. Let us use our leadership to focus on what unites us. Let’s be sure that when it comes to the American Academy of Otolaryngology–Head and Neck Surgery that the whole is much greater than the sum of its parts.
 David R. Nielsen, MD AAO-HNS/F EVP/CEO
David R. Nielsen, MD AAO-HNS/F EVP/CEOEach October signals the tenure of a new round of Academy leadership. Not only do we inaugurate and honor a new Academy president, but a significant number of board members of both the Academy and the Foundation, as well as committee members and chairs, turn over each year. As I reflect on the “changing of the guard,” I experience two strong emotional responses. First, I am continually amazed and honored to be allowed to work so closely with such effective, selfless, and dedicated leadership. Working so closely with these remarkable men and women inspires me with confidence for the future. It is reassuring to know that we have an endless supply of talent and inspirational leadership.
Second, my gratitude for the voluntary service represented by these leaders (emblematic of the culture of service that pervades our entire membership) is hard to put into words. So it is with great thanks and some sadness that we say “thank you” to James L. Netterville, MD, for his very personable, gracious, and effective leadership during the last year, and welcome with enthusiasm and anticipation the energy and guidance of our new president, Richard W. Waguespack, MD. As you all know, for nearly two decades we have alternated the selection of many of our officers, board, and committees members between community-based and academic otolaryngologists. In that manner, directly elected board directors, Nominating Committee members, as well as the president always bring the perspective of our entire membership, not just a popular or more vocal segment, to the table.
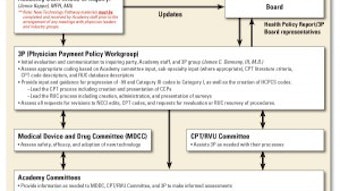
This is a timely reminder, since this October issue of the Bulletin devotes focus to our membership and several committees. The structure of our Boards of Directors, the BOG, and our relationship with state, regional, or other specialty societies is designed to strike the optimal balance between the common ground that unites all of us as otolaryngologists and the desired autonomy of smaller societies who effectively provide community, subspecialty, or other interest or focus.
The manner in which humans organize themselves to achieve things together that they could not achieve alone makes for interesting study. Whether forming a new neighborhood tree house club or a new nation, humans have sought safety, camaraderie, solace, community, or collective action with likeminded people since before recorded history. While the consequences of the boundaries we formally place around our relationships, and the number of “groups” we feel a kinship with has a serious impact on many aspects of our lives, some of what we learn over time makes us ask, “What were they thinking?” (Or, perhaps more to the point, “What were we thinking?!”) In his book, How the States Got Their Shapes, Mark Stein comments on the tremendous insight to be gained from researching this question. “Far more knowledge results from exploring why a set of conditions exists than from simply accepting those conditions and committing them to memory. Asking why a state has the borders it does unlocks a history of human struggles–far more history…” than the question implies. In studying why our geographic boundaries are the way they are, we learn about politics, war, grants, gifts, generosity, forgiveness, complaisance, incompetence, resignation, and regret. We discover the challenge of overcoming the inertia of culture, the bonds of familiarity, and the fear of the uncertain.
These ideas are affecting how we move forward as otolaryngologists in both our internal and external environments. Internally, we have for years benefited from addressing the challenge of asking why we are organized the way we are, why we do things the way we do, and are our traditions, assumptions, and expectations still valid and relevant. We are drafting an entirely new version of our Member Handbook, complete with standard operating procedures, documentation of processes, and accurate and updated application of bylaws, policies, and positions that benefit our members, and by extension, our patients. Externally, we are being forced by economics, politics, and our professional desire to be the best to challenge foundational assumptions of how we organize healthcare, delivery and payment models, and methods for ensuring the highest quality of care can be delivered with the most effective utilization of resources.
As we return to our practices after another successful Annual Meeting & OTO EXPOSM, let us meet the challenge to bring out the best in each other, professionally, personally, and organizationally. Let us use our leadership to focus on what unites us. Let’s be sure that when it comes to the American Academy of Otolaryngology–Head and Neck Surgery that the whole is much greater than the sum of its parts.