Optum: An Academy Advantage Partner—A Proactive Treatment Plan Addressing ICD-10-CM “Code Z56.5”*
According to the most recent ICD-10-CM/PCS implementation timeline released by the Centers for Medicare & Medicaid Services (CMS), small, medium, and large practices should already have conducted high-level training on ICD-10-CM for clinicians and coders. To stay on track with the timeline, those practices should currently be testing clinical documentation, coding practices, software, and billing, with October 2013 as the time for practices to begin testing claim transactions with business partners. January 1–April 1, 2014, is the designated time to review coder and clinician preparation with detailed ICD-10-CM coding training. There will be no further delays, and the implementation date is firmly October 1, 2014, for all healthcare providers. For the otolaryngologist, this new generation of coding will facilitate the capture of much greater specificity and clinical information, resulting in increased sensitivity when refining diagnosis grouping and establishing reimbursement methodologies. Plus, better coded data improves clinical decision making and outcomes measurement. While the challenges of coding with ICD-10-CM for otolaryngology are perhaps less significant than for other specialties, they still exist. So what are the steps you can take now to avoid the condition described by ICD-10-CM code Z56.5?* Step 1: Relax, most of the significant changes: code expansion, coding guidance, coding instruction, and classification axes have, for the most part, left the most commonly assigned codes in otolaryngology unscathed. That’s not to imply that solid coding training and preparation can be ignored. Coding training and documentation improvements are necessary to achieve coding compliance. What is important is that this advantage of fewer changes provides a head start in several ways. First, the historical ICD-9-CM coded data will be more easily mapped to ICD-10-CM and will continue to provide valuable data. Second, documentation improvement necessary for coding will not be a giant leap. Third, coding training can be focused, and risks associated with delayed claim submission and denials can be avoided. Step 2: Initiate the action plan for real-time coding training. Appoint an ICD-10-CM coding trainer to take the lead in this action plan. Identify a critical subset of ICD-9-CM codes based on utilization/reimbursement assessment. Code the subset of diagnoses using ICD-10-CM. Mapping can assist in this task as long as it is used in combination with code set knowledge, anatomy and physiology fundamentals, and proper coding practices. Identify any differences in clinical concepts, classification axes, coding practices, and terminology for the specific subset of codes. Assess and implement documentation improvement and coding practices concerning the identified coding differences required for accurate code assignment. Focus ICD-10-CM training based on the code utilization subset including the clinical concepts, classification axes, coding practices, and terminology challenges for the subset of codes. Assess skill levels after training and institute periodic refresher training and coding issue discussions. Step 3: Address these coding/documentation issues challenges. Aftercare versus subsequent encounter: Aftercare visit codes cover situations when the initial treatment of a disease has been performed and the patient requires continued care during the healing or recovery phase or for the long-term consequences of the disease. Subsequent encounter codes cover encounters after the patient has received active treatment for the injury and is receiving routine care for that injury. Laterality: right, left, and bilateral options Asthma: mild intermittent, mild persistent, moderate persistent, and severe persistent classification Recurrent versus nonrecurrent episodes of infections Step 4: Create a work environment that embraces a positive attitude toward change, and thus avoid unnecessary stressors associated with a change as fundamental as a new coding classification system. Taking the steps outlined above will provide a solid foundation for transitioning to ICD-10-CM and avoid the condition described by Z56.5. *Z56.5 Uncongenial work environment (Difficult conditions at work)

For the otolaryngologist, this new generation of coding will facilitate the capture of much greater specificity and clinical information, resulting in increased sensitivity when refining diagnosis grouping and establishing reimbursement methodologies. Plus, better coded data improves clinical decision making and outcomes measurement.
While the challenges of coding with ICD-10-CM for otolaryngology are perhaps less significant than for other specialties, they still exist. So what are the steps you can take now to avoid the condition described by ICD-10-CM code Z56.5?*

Relax, most of the significant changes: code expansion, coding guidance, coding instruction, and classification axes have, for the most part, left the most commonly assigned codes in otolaryngology unscathed. That’s not to imply that solid coding training and preparation can be ignored. Coding training and documentation improvements are necessary to achieve coding compliance. What is important is that this advantage of fewer changes provides a head start in several ways. First, the historical ICD-9-CM coded data will be more easily mapped to ICD-10-CM and will continue to provide valuable data. Second, documentation improvement necessary for coding will not be a giant leap. Third, coding training can be focused, and risks associated with delayed claim submission and denials can be avoided.
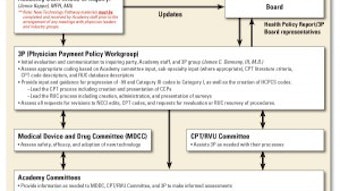
Step 2:
Initiate the action plan for real-time coding training.
- Appoint an ICD-10-CM coding trainer to take the lead in this action plan.
- Identify a critical subset of ICD-9-CM codes based on utilization/reimbursement assessment.
- Code the subset of diagnoses using ICD-10-CM. Mapping can assist in this task as long as it is used in combination with code set knowledge, anatomy and physiology fundamentals, and proper coding practices.
- Identify any differences in clinical concepts, classification axes, coding practices, and terminology for the specific subset of codes.
- Assess and implement documentation improvement and coding practices concerning the identified coding differences required for accurate code assignment.
- Focus ICD-10-CM training based on the code utilization subset including the clinical concepts, classification axes, coding practices, and terminology challenges for the subset of codes.
- Assess skill levels after training and institute periodic refresher training and coding issue discussions.
Step 3:
Address these coding/documentation issues challenges.
- Aftercare versus subsequent encounter:
- Aftercare visit codes cover situations when the initial treatment of a disease has been performed and the patient requires continued care during the healing or recovery phase or for the long-term consequences of the disease.
- Subsequent encounter codes cover encounters after the patient has received active treatment for the injury and is receiving routine care for that injury.
- Laterality: right, left, and bilateral options
- Asthma: mild intermittent, mild persistent, moderate persistent, and severe persistent classification
- Recurrent versus nonrecurrent episodes of infections
Step 4:
Create a work environment that embraces a positive attitude toward change, and thus avoid unnecessary stressors associated with a change as fundamental as a new coding classification system. Taking the steps outlined above will provide a solid foundation for transitioning to ICD-10-CM and avoid the condition described by Z56.5.
*Z56.5 Uncongenial work environment (Difficult conditions at work)