International Consensus Statement on Allergy and Rhinology: Allergic Rhinitis 2023
Important recommendations that may change our practice.
Sarah Wise, MD (Member), Lauren Roland, MD (Member), Cecelia Damask, DO (Chair), and Joshua Levy, MD (Member), Allergy, Asthma, and Immunology Committee

Inertia exists in medical practice. Inertia is often the reason that clinicians continue to offer the same advice to patients or prescribe the same treatment, even if evidence has changed. Reading extensive published research, systematic reviews, and guidelines is a monumental task. And changing clinical practice to adopt new approaches can sometimes seem like an insurmountable undertaking. But inertia can be overcome. Small incremental changes can offer a path toward overcoming inertia and implementation of sustainable positive changes over time.
Published literature on allergic rhinitis (AR) has expanded substantially in recent decades. A PubMed search performed in 2022, identified 7,169 citations concerning AR published from 2018 to 2022. This daunting amount of new literature may be overwhelming for the busy clinician and contribute to inertia. Fortunately, there was a document published in early 2023 that can aid otolaryngologists in tackling this formidable mountain of evidence.
International Consensus Statement on Allergy and Rhinology: Allergic Rhinitis - 20231 (ICAR: AR – 2023) is a tool that otolaryngologists can quickly and easily reference on numerous topics related to AR (Table 1). ICAR: AR – 2023 included the participation of over 120 authors who critically appraised the evidence on 144 individual topics within 10 major content areas surrounding AR. This document also provides guidance for clinicians using the evidence-based review with recommendations (EBRR) methodology. Major content areas include the definition of AR and differential diagnosis, pathophysiology, epidemiology, disease burden, risk and protective factors, evaluation and diagnosis, management (including aeroallergen avoidance and environmental controls, single and combination pharmacotherapy options, allergen immunotherapy), pediatric considerations, associated conditions, and a special section on COVID-19. There are 41 new AR topics evaluated in ICAR: AR – 2023 compared to original ICAR:AR – 2018.2 Furthermore, by extensively evaluating the AR literature, knowledge gaps and unmet needs become evident—these are also addressed in ICAR: AR – 2023. We highlight some of the new information below.
Table 1. International Consensus Statement on Allergy and Rhinology: Allergic Rhinitis - 2023.
 Source: Wise SK, Damask C, Roland LT, Ebert C, Levy JM, et al. International consensus statement on allergy and rhinology: Allergic rhinitis - 2023. Int Forum Allergy Rhinol. 2023 Apr;13(4):293-859.
Source: Wise SK, Damask C, Roland LT, Ebert C, Levy JM, et al. International consensus statement on allergy and rhinology: Allergic rhinitis - 2023. Int Forum Allergy Rhinol. 2023 Apr;13(4):293-859.
Epidemiology
The prevalence of AR is reported between 5% and 50% worldwide, with incidence increasing in childhood until early adulthood. Prevalence varies by geographical location and latitude and is highest in English speaking countries. The effect of climate change on AR prevalence is being studied.3
Diagnostics
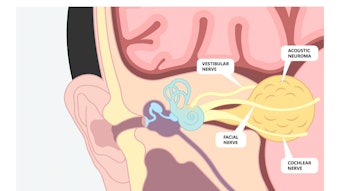
History is critical to AR diagnosis. There are several validated survey and quality of life tools that can aid in diagnosis. Physical exam includes nasal endoscopy as an optional tool, which may reveal central compartment edema or polypoid changes that have recently been associated with allergy.4 Nasal endoscopy can also help rule out other more concerning diagnoses. Confirmatory testing is helpful when considering targeted avoidance strategies or allergen immunotherapy, which may be beneficial when medical therapy is not satisfactory in controlling symptoms.
Skin prick testing (SPT) is recommended when the diagnosis of AR needs to be confirmed or in a patient with presumed AR who has failed appropriate empiric medical therapy and allergen immunotherapy (AIT) is being considered. Intradermal and blended techniques are considered options for confirming allergic sensitization. Serum allergen-specific IgE testing is also a recommended testing modality and may be necessary when patients have relative or absolute contraindications to skin testing, such as beta-blocker use, uncontrolled asthma, or medication use that may interfere with the skin test response.
Treatment options
Avoidance
Although commonly employed in AR management, the evidence surrounding most allergen avoidance strategies is mixed. Optional interventions include pet, pest, and pollen allergen avoidance measures.
Medications
Strong recommendations for AR treatment include a recommendation for the use of the following:
- Newer generation oral antihistamines compared with first-generation alternatives
- Intranasal corticosteroids
- Intranasal saline
- Combination therapy with intranasal corticosteroid plus intranasal antihistamine for patients not responding to monotherapy
- Subcutaneous immunotherapy [SCIT] or sublingual immunotherapy [SLIT] tablets in properly selected patients.
There is also a strong recommendation against the use of oral decongestant monotherapy and the routine use of oral corticosteroids for AR treatment.
Immunotherapy
SCIT for AR is a treatment option with a strong recommendation and high certainty of evidence. SCIT is an effective therapeutic intervention, as reflected in improvements in symptoms and quality of life (QOL), along with decreased rescue medication use. SLIT has also been shown to be efficacious, with symptom and QOL improvement, as well as decreased reliance on medications. Meta-analyses have shown superior efficacy of SCIT, although these findings were based largely on indirect comparisons, and found a safety advantage of SLIT compared with SCIT.
Pediatrics
In the pediatric population, it is important to consider the “allergic march” and evaluate for a family history of atopy. Skin prick testing is commonly performed in children. Although treatment options are limited for very young children, allergen immunotherapy may reduce the risk of development of asthma later in life in children with AR.
Associated Conditions
Due to the unified airway, there is a well-accepted association of asthma with AR, and AR is a risk factor for asthma development. In patients with both AR and asthma, treatment with allergen immunotherapy improves asthma symptoms in addition to AR symptoms. Additionally, the relationship of AR to several forms of chronic rhinosinusitis has been investigated.
Although studies are mixed, allergy is thought to play a role in allergic fungal rhinosinusitis and central compartment atopic disease. Although there is increased prevalence of IgE-mediated allergy in aspirin-exacerbated respiratory disease in recent reports compared to original reports, the primary pathophysiology of aspirin-exacerbated respiratory disease lies in altered arachidonic acid metabolism rather than IgE-mediated hypersensitivity. There is fairly strong data for an association of sleep disturbance, pollen food allergy syndrome, conjunctivitis and atopic dermatitis with AR.
COVID-19
The COVID-19 pandemic initially caused several challenges with diagnosis and management of AR due to concerns for healthcare provider safety. There was also motivation to control allergic symptoms to avoid spread of COVID-19 through sneezing and other hallmark AR symptoms. Although studies are limited, standard AR treatment is not contraindicated in COVID-19 patients. Additionally, immunotherapy is considered safe. Initiation of allergen immunotherapy was not recommended during quarantine and times of high caseloads of COVID-19, and consideration to SLIT was given for convenience.
Areas of Future Research
There are several areas of research that need to be addressed regarding AR. Risk factors for development of AR and the relationship of risk factors to genetics remains poorly understood. The role of climate change, weather, and geography on AR development is also an ongoing area of work.
Cost-effective testing options for AR are also under investigation, such as nasal allergen-specific IgE and mast cell activation levels. For treatment, combination therapies and head-to-head cost and efficacy comparisons of available options, such as SLIT and SCIT, are needed. Lastly, an improved understanding of the effects of AR on other otolaryngic diseases, such as nasal polyps, ear disease, and voice disorders, is warranted for improved treatment of head and neck disease in general.
Change is integral in our efforts to provide the best possible outcomes for our patients. By working together, the authors of ICAR: AR – 2023 have provided us with a valuable tool we can use to overcome inertia and achieve and sustain the best outcomes for our patients in the management of AR.
“If everyone is moving forward together, then success takes care of itself.”
- Henry Ford
References
- Wise SK, Damask C, Roland LT, Ebert C, Levy JM, et al. International consensus statement on allergy and rhinology: Allergic rhinitis - 2023. Int Forum Allergy Rhinol. 2023 Apr;13(4):293-859.
- Wise SK, Lin SY, Toskala E, Orlandi RR, Akdis CA, et al. International Consensus Statement on Allergy and Rhinology: Allergic Rhinitis. Int Forum Allergy Rhinol. 2018 Feb;8(2):108-352.
- Wise SK, Damask C, Greenhawt M, Oppenheimer J, Roland LT, Shaker MS, Wallace DV, Lang DM. A Synopsis of Guidance for Allergic Rhinitis Diagnosis and Management From ICAR 2023. J Allergy Clin Immunol Pract. 2023 Mar;11(3):773-796.
- DelGaudio JM, Loftus PA, Hamizan AW, Harvey RJ, Wise SK. Central compartment atopic disease. Am J Rhinol Allergy. 2017 Jul 1;31(4):228-234.