Reg-ent Growth
Now in its sixth year, the Reg-ent registry has soundly endured as the only national otolaryngology-specific data repository, one that is solely focused on the specialty of otolaryngology-head and neck surgery, its physicians, and its patients.

Reg-ent participants engage with their data and are actively involved in mapping refinement and data validation of Reg-ent quality measures, which include 11 otolaryngology-specific measures designed by and for AAO-HNS members and available only in Reg-ent. Reg-ent participants are also committed to the success of the registry, which is evident by the increase in renewal rates in Reg-ent with many renewing practices adding more clinicians to the registry. This commitment to the registry—and to the future of the specialty—is shown by the continued participation of existing practices and the growth in Reg-ent as it adds new private practices and new academic medical centers.
Research
Building on these significant achievements, Reg-ent has now entered its next phase of development, data analytics, and research. Reg-ent has partnered with OM1 for data curation and analytics. OM1 is ingesting data from Reg-ent, which will ultimately lead to research capabilities as well as clinical trial opportunities through OM1. Once the data are curated to research grade, OM1 will be able to create deidentified data sets that will be accessible through an online research platform. Research-focused policies and procedures will be utilized by the Reg-ent Research Advisory Group (RRAG), chaired by Vikas Mehta, MD, MPH, Coordinator for Research and Quality, to guide potential investigators and to prioritize research data requests. Future growth for the Reg-ent registry will focus on optimizing the value of the Reg-ent registry.
The AAO-HNSF has invested in the infrastructure for data curation, advanced data analytics, and research. The power of the registry is in the data—the greater number of participants, the more data we collect, and the more we can optimize the power of the data for research, advocacy, and defining quality care. We encourage all members to invest in Reg-ent, the most significant quality improvement initiative of the AAO-HNSF. Participants in similar specialty-based registries have realized financial benefits from their participation as the aggregate data has been used to value treatment options and allow for clinical trial participation, as well as to provide data to support advocacy efforts.
Assessing and Forecasting the Financial Impact of MIPS
As Reg-ent continues to expand in its capabilities into research and data analytics, benefiting all members regardless of practice setting, it also continues to recognize the value of CMS quality reporting to many of our members and their practices. Over the past two years amid the pandemic, participating sites have maintained engagement with Reg-ent and their data, with approximately 1,250 clinicians using Reg-ent to report some or all three categories of the Merit-based Incentive Payment System (MIPS) for the 2021 performance year.
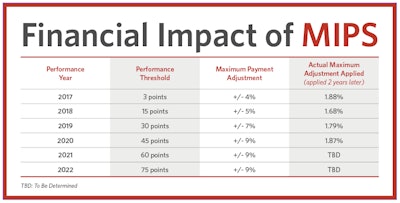
Since the inception of the MIPS program, the threshold to achieve a positive payment adjustment has increased each year. In the 2017 performance year, the payment adjustment was 4% with minimal requirements and 3-point performance threshold to avoid a negative impact. Earning a positive payment adjustment is increasingly difficult, as indicated in the table on page 28.
For the 2022 performance year, the payment adjustment rose to 9% with a 75-point performance threshold. In addition to the increased performance threshold, CMS eliminated bonus points for end-to-end reporting or submitting of additional outcome or high-priority measures.
High performers within MIPS continue to be underwhelmed by low payment adjustments for exceptional scores. The maximum positive adjustment for exceptional scores was 1.87% in the 2022 payment year. Under the 2015 MACRA legislation, MIPS is required to be “budget neutral”—the projected negative adjustments must be balanced by the projected positive adjustments. With so many clinicians successfully participating, the distribution of positive adjustments is spread thinner. Another factor perhaps affecting the distribution of positive payments is the COVID-19 pandemic and CMS’s Extreme and Uncontrollable Circumstances (EUC) exception for COVID-19. During the 2020 and 2021 performance years and subsequent 2022 payment year adjustment, individually eligible MIPS clinicians who did not submit any data received a neutral payment adjustment instead of the maximum negative adjustment that would have applied in 2019 and earlier. With the new threshold requirements and perceived retirement of previous automatic COVID-19 EUCs, it will be harder to earn positive or exceptional performances. With presumably fewer clinicians on the positive side of the budget-neutral ring, there may be greater financial reward than in previous years.
With the increased performance threshold, many clinicians may need to rethink their approach to meet MIPS standards for quality, improvement activities, Promoting Interoperability, and cost. The latest publication of the Quality Payment Program (QPP) Experience data set provides performance scores and associated payment adjustments for the 2018 performance year (threshold of 15 points). If included clinicians earned the same scores in performance year 2022, approximately one in six clinicians who received a positive adjustment for the 2018 performance year will move to a negative adjustment for 2022. Specialty-wise, this trend extends to one in seven allergists/immunologists and one in eight otolaryngologists stating the 2019 QPP Experience Report was not available at the time.
Reg-ent is deploying strategies to optimize MIPS scores by (1) assisting Reg-ent participants to select measures with maximum scoring potential, (2) reducing mapping burden, (3) collaborating with EHRs to expand available measures, and (4) encouraging specialty quality measure reporting to create benchmarks that raise point ceilings. Reg-ent will continue to engage practices to prepare for other MIPS performance categories, improvement activities and Promoting Interoperability, to deploy initiatives that will improve final scores. AAO-HNSF continues to request greater transparency from CMS for the cost performance category.
Through participation in Reg-ent and contribution of data to the registry, members are individually and collectively impacting the future of the specialty in a positive and invaluable way. We continue to bring aboard new members and their practices and look forward to the continued growth, development, and diversification of the Reg-ent registry.