Chronic Ear Disease in Zanzibar
Mark E. Zafereo, Jr, MD Chair, Section for Residents and Fellows MD Anderson, Houston, TX Tanzania has only eight otolaryngologists to serve a population of 40 million people. Zanzibar, a semi-autonomous tropical island located 20 miles off the east coast of Tanzania, with a population of about one million people, has just a single otolaryngologist. The World Health Organization estimates Tanzania to be among the countries with the highest prevalence (more than 4 percent) of chronic suppurative otitis media (CSOM), requiring “urgent attention needed to deal with a massive public health problem.”1 In addition to higher prevalence, CSOM has been reported to result in more severe conductive hearing loss in the Tanzanian population.2 A large number of adolescents suffer with sequelae of CSOM, including subtotal perforations, ossicular chain erosion, and significant conductive hearing loss. Through collaboration between Global ENT Outreach (GEO) and IMPACT United Kingdom, we conducted a one-week otology course at Mnazi Mmoja Hospital, Zanzibar, Tanzania. Our team was led by Richard Wagner, MD, founder and acting director of GEO, and included three other physicians (Marta Sandoval, MD, Charles Z. Weingarten, MD, and myself), and one medical educator, Giuliana Duret. Over five days, we performed 39 otologic surgeries, predominantly tympanoplasties and ossicular chain reconstructions in adolescents with a history of CSOM during childhood and resultant conductive hearing loss due to tympanic membrane perforations and ossicular chain erosions. Interestingly, none of these patients had cholesteatomas, consistent with previously published reports of low incidence of cholesteatoma in this region.2,3 During the five-day course, we trained two Tanzanian otolaryngologists, Naufal Kassim Mohammed, MD, and Edwin Liyombo, MD, in the techniques of tympanoplasties and ossicular chain reconstructions. We instructed them in both transcanal and retroauricular approaches, as well as both medial and lateral grafting techniques, with all surgeries televised to optimize teaching opportunities. Although the Tanzanian otolaryngologists had little previous experience with tympanoplasties, their confidence increased throughout the week. By the last day of the course, they could perform simple tympanoplasties with little need for instruction. At the conclusion of the trip, we evaluated our experience and impact. We were surprised by the paucity of cholesteatomas in this population of patients with chronic middle ear disease. All patients were referred from the Zanzibar Outreach Program (ZOP), an educational and preventive effort which includes screening evaluations for chronic ear disease in schools on the island. Therefore, all patients who were evaluated during the five-day otology course were older children and adolescents, and there could potentially be some selection bias in this process. However, Dr. Mohammed, ZOP coordinator and the only otolaryngologist on the island, notes that he sees only about one cholesteatoma a year. Most of the perforations we saw were large, dry, central perforations; we hypothesized that cholesteatomas were less prevalent in this population due to genetics, or perhaps because the temperate climate results in fewer upper respiratory infections. In contrast to a recent GEO trip to Ethiopia, where most surgeries were performed for extensive and potentially life-threatening cholesteatomas, all 39 surgeries in Tanzania were elective. Reflecting on the resource use of performing elective surgeries (tympanoplasties and ossicular chain reconstructions) in the developing world, we wondered if efforts and resources would be better allocated to procedures with potential life-saving benefit. In general, in the developed world in which we live, otology is mainly about quality of life, while in the developing world with fewer resources, otologists perhaps should focus more on prevention and efforts that will save lives. Nevertheless, we were grateful for the opportunity to improve the quality of life of a small population of patients, provide community education, and share our knowledge with two eager Tanzanian otolaryngologists. References Acuin, J. Chronic Suppurative Otitis Media: Burden of Illness and Management Options. World Health Organization. 2004. Geneva, Switzerland. Manni JJ, Lema PN. Otitis media in Dar es Salaam, Tanzania. J Laryngol Otol. 1987;101: 222-8. Roland, PE. Otological problems in Uganda. J Laryngolo Otol. 1960;74:678-84.
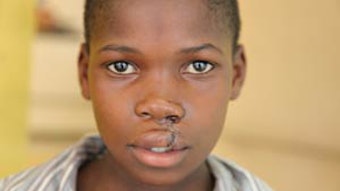
 Group picture of surgeons, anesthesiologists, and operating room nursing staff outside the operating room on the last day of the ear surgery course at Mnazi Mmoja hospital in Zanzibar, Tanzania. (Dr. Zafereo at top left).
Group picture of surgeons, anesthesiologists, and operating room nursing staff outside the operating room on the last day of the ear surgery course at Mnazi Mmoja hospital in Zanzibar, Tanzania. (Dr. Zafereo at top left).Mark E. Zafereo, Jr, MD
Chair, Section for Residents and Fellows
MD Anderson, Houston, TX
Tanzania has only eight otolaryngologists to serve a population of 40 million people. Zanzibar, a semi-autonomous tropical island located 20 miles off the east coast of Tanzania, with a population of about one million people, has just a single otolaryngologist.
The World Health Organization estimates Tanzania to be among the countries with the highest prevalence (more than 4 percent) of chronic suppurative otitis media (CSOM), requiring “urgent attention needed to deal with a massive public health problem.”1 In addition to higher prevalence, CSOM has been reported to result in more severe conductive hearing loss in the Tanzanian population.2 A large number of adolescents suffer with sequelae of CSOM, including subtotal perforations, ossicular chain erosion, and significant conductive hearing loss.
Through collaboration between Global ENT Outreach (GEO) and IMPACT United Kingdom, we conducted a one-week otology course at Mnazi Mmoja Hospital, Zanzibar, Tanzania. Our team was led by Richard Wagner, MD, founder and acting director of GEO, and included three other physicians (Marta Sandoval, MD, Charles Z. Weingarten, MD, and myself), and one medical educator, Giuliana Duret. Over five days, we performed 39 otologic surgeries, predominantly tympanoplasties and ossicular chain reconstructions in adolescents with a history of CSOM during childhood and resultant conductive hearing loss due to tympanic membrane perforations and ossicular chain erosions. Interestingly, none of these patients had cholesteatomas, consistent with previously published reports of low incidence of cholesteatoma in this region.2,3
During the five-day course, we trained two Tanzanian otolaryngologists, Naufal Kassim Mohammed, MD, and Edwin Liyombo, MD, in the techniques of tympanoplasties and ossicular chain reconstructions. We instructed them in both transcanal and retroauricular approaches, as well as both medial and lateral grafting techniques, with all surgeries televised to optimize teaching opportunities. Although the Tanzanian otolaryngologists had little previous experience with tympanoplasties, their confidence increased throughout the week. By the last day of the course, they could perform simple tympanoplasties with little need for instruction.
At the conclusion of the trip, we evaluated our experience and impact. We were surprised by the paucity of cholesteatomas in this population of patients with chronic middle ear disease. All patients were referred from the Zanzibar Outreach Program (ZOP), an educational and preventive effort which includes screening evaluations for chronic ear disease in schools on the island. Therefore, all patients who were evaluated during the five-day otology course were older children and adolescents, and there could potentially be some selection bias in this process. However, Dr. Mohammed, ZOP coordinator and the only otolaryngologist on the island, notes that he sees only about one cholesteatoma a year. Most of the perforations we saw were large, dry, central perforations; we hypothesized that cholesteatomas were less prevalent in this population due to genetics, or perhaps because the temperate climate results in fewer upper respiratory infections.
In contrast to a recent GEO trip to Ethiopia, where most surgeries were performed for extensive and potentially life-threatening cholesteatomas, all 39 surgeries in Tanzania were elective. Reflecting on the resource use of performing elective surgeries (tympanoplasties and ossicular chain reconstructions) in the developing world, we wondered if efforts and resources would be better allocated to procedures with potential life-saving benefit.
In general, in the developed world in which we live, otology is mainly about quality of life, while in the developing world with fewer resources, otologists perhaps should focus more on prevention and efforts that will save lives. Nevertheless, we were grateful for the opportunity to improve the quality of life of a small population of patients, provide community education, and share our knowledge with two eager Tanzanian otolaryngologists.
References
- Acuin, J. Chronic Suppurative Otitis Media: Burden of Illness and Management Options. World Health Organization. 2004. Geneva, Switzerland.
- Manni JJ, Lema PN. Otitis media in Dar es Salaam, Tanzania. J Laryngol Otol. 1987;101: 222-8.
- Roland, PE. Otological problems in Uganda. J Laryngolo Otol. 1960;74:678-84.