AMA Adopts Principles on Accountable Care Organizations
Liana Puscas, MD Chair, AAO-HNS Delegation The American Medical Association (AMA) held its interim meeting in November 2010. Our Academy was represented by Liana Puscas, MD, delegation chair; delegates Michael S. Goldrich, MD, Shannon Pryor, MD, and Robert Puchalski, MD; alternate delegate David R. Nielsen, MD, AAO-HNS EVP/CEO; and Academy staff. The AMA debated at length the issue of federally mandated individual purchase of health insurance, ultimately deciding to study the problem further before agreeing to a specific policy. While a mandate with palpable penalties for non-compliance would have the benefit of increasing the number of Americans with health insurance and is a necessary element of broader health insurance reforms, the principle of individual federal mandates rankled many delegates because of the accompanying increased involvement of government in medicine and the reality that insurance coverage alone does not guarantee access to healthcare (e.g., paucity of physicians who accept Medicaid). A significant portion of the debate revolved around the concept of using tax credits or tax penalties as a more palatable way of encouraging individuals to obtain health insurance. The House of Delegates also voted to study the use of tax credits and other mechanisms to aid physicians who provide un- or under-compensated care. Of specific importance to our specialty, the AMA supported the addition of interpreters for hearing-impaired patients to its study on the impact of any federal mandate that requires an interpreter to be present for patients who cannot communicate proficiently in English. One of the most significant actions was the adoption of principles that should guide the development of accountable care organizations (ACOs). According to CMS’s definition, an ACO is an organization of healthcare providers that agrees to be accountable for the quality, cost, and overall care of Medicare beneficiaries enrolled in the traditional fee-for-service program who are assigned to it. (“Assigned” means those beneficiaries for whom the professionals in the ACO provide the bulk of primary care services.) Assignment will not affect the beneficiaries’ guaranteed benefits or choice of doctor. Overall, the AMA’s principles emphasize that ACOs must be physician-led, place patients’ interests first, ensure voluntary physician and patient participation, and enable independent physicians to participate. The following is an edited version of the principles: Guiding Principle – The goal of an ACO is to increase access to care, improve the quality of care, and ensure the efficient delivery of care. Within an ACO, a physician’s primary ethical and professional obligation is the well-being and safety of the patient. ACO Governance – ACOs must be physician-led and encourage an environment of collaboration among physicians. Physician and patient participation in an ACO should be voluntary. Physicians should not be required to join an ACO as a condition of contracting with Medicare, Medicaid, or a private payer or being admitted to a hospital medical staff. The savings and revenues of an ACO should be retained for patient care services and distributed to ACO participants. Flexibility is necessary in patient referral and antitrust laws to allow physicians to collaborate with hospitals in forming ACOs without being employed by the hospitals or ACOs. Additional resources (grants) should be provided up-front in order to encourage ACO development. The ACO spending benchmark, which will be based on historical spending patterns in the ACO’s service area and negotiated between Medicare and the ACO, should be adjusted for differences in geographic practice costs and risk adjusted for individual patient risk factors. The quality performance standards required to be established by the Secretary of HHS must be consistent with existing AMA policy regarding quality, including the use of nationally accepted, physician specialty-validated clinical measures developed by the AMA-specialty society quality consortium (of which our Academy is a part). An ACO must be afforded due process with respect to the Secretary of HHS’s discretion to terminate an agreement with an ACO for failure to meet the quality performance standards. ACOs should be allowed to use different payment models, including fee-for-service, capitation, partial capitation, medical homes, care management fees, and shared savings plans. The Consumer Assessment of Healthcare Providers and Systems (CAHPS) Patient Satisfaction Survey should be used as a tool to determine patient satisfaction and whether an ACO meets the patient-centeredness criteria required by the ACO law. Interoperable Health Information Technology and Electronic Health Record Systems are keys to the success of ACOs. The ACO must abide by the financial solvency standards pertaining to risk-bearing organizations.
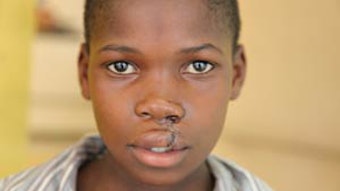
Liana Puscas, MD
Chair, AAO-HNS Delegation
The American Medical Association (AMA) held its interim meeting in November 2010. Our Academy was represented by Liana Puscas, MD, delegation chair; delegates Michael S. Goldrich, MD, Shannon Pryor, MD, and Robert Puchalski, MD; alternate delegate David R. Nielsen, MD, AAO-HNS EVP/CEO; and Academy staff.
The AMA debated at length the issue of federally mandated individual purchase of health insurance, ultimately deciding to study the problem further before agreeing to a specific policy. While a mandate with palpable penalties for non-compliance would have the benefit of increasing the number of Americans with health insurance and is a necessary element of broader health insurance reforms, the principle of individual federal mandates rankled many delegates because of the accompanying increased involvement of government in medicine and the reality that insurance coverage alone does not guarantee access to healthcare (e.g., paucity of physicians who accept Medicaid).
A significant portion of the debate revolved around the concept of using tax credits or tax penalties as a more palatable way of encouraging individuals to obtain health insurance. The House of Delegates also voted to study the use of tax credits and other mechanisms to aid physicians who provide un- or under-compensated care. Of specific importance to our specialty, the AMA supported the addition of interpreters for hearing-impaired patients to its study on the impact of any federal mandate that requires an interpreter to be present for patients who cannot communicate proficiently in English.
One of the most significant actions was the adoption of principles that should guide the development of accountable care organizations (ACOs). According to CMS’s definition, an ACO is an organization of healthcare providers that agrees to be accountable for the quality, cost, and overall care of Medicare beneficiaries enrolled in the traditional fee-for-service program who are assigned to it. (“Assigned” means those beneficiaries for whom the professionals in the ACO provide the bulk of primary care services.) Assignment will not affect the beneficiaries’ guaranteed benefits or choice of doctor.
Overall, the AMA’s principles emphasize that ACOs must be physician-led, place patients’ interests first, ensure voluntary physician and patient participation, and enable independent physicians to participate.
The following is an edited version of the principles:
- Guiding Principle – The goal of an ACO is to increase access to care, improve the quality of care, and ensure the efficient delivery of care. Within an ACO, a physician’s primary ethical and professional obligation is the well-being and safety of the patient.
- ACO Governance – ACOs must be physician-led and encourage an environment of collaboration among physicians.
- Physician and patient participation in an ACO should be voluntary. Physicians should not be required to join an ACO as a condition of contracting with Medicare, Medicaid, or a private payer or being admitted to a hospital medical staff.
- The savings and revenues of an ACO should be retained for patient care services and distributed to ACO participants.
- Flexibility is necessary in patient referral and antitrust laws to allow physicians to collaborate with hospitals in forming ACOs without being employed by the hospitals or ACOs.
- Additional resources (grants) should be provided up-front in order to encourage ACO development.
- The ACO spending benchmark, which will be based on historical spending patterns in the ACO’s service area and negotiated between Medicare and the ACO, should be adjusted for differences in geographic practice costs and risk adjusted for individual patient risk factors.
- The quality performance standards required to be established by the Secretary of HHS must be consistent with existing AMA policy regarding quality, including the use of nationally accepted, physician specialty-validated clinical measures developed by the AMA-specialty society quality consortium (of which our Academy is a part).
- An ACO must be afforded due process with respect to the Secretary of HHS’s discretion to terminate an agreement with an ACO for failure to meet the quality performance standards.
- ACOs should be allowed to use different payment models, including fee-for-service, capitation, partial capitation, medical homes, care management fees, and shared savings plans.
- The Consumer Assessment of Healthcare Providers and Systems (CAHPS) Patient Satisfaction Survey should be used as a tool to determine patient satisfaction and whether an ACO meets the patient-centeredness criteria required by the ACO law.
- Interoperable Health Information Technology and Electronic Health Record Systems are keys to the success of ACOs.
- The ACO must abide by the financial solvency standards pertaining to risk-bearing organizations.