Controversy in Coding for Vestibular Schwannoma Surgery
Designating CPT codes for skull base surgeries serves as a cautionary tale for attempting to establish or modify codes for other procedures.
Pamela Roehm, MD, PHD, Chair, Rick Nelson, MD, PhD, Mark Wiet, MD, Shawn Stevens, MD, AAO-HNS Skull Base Surgery Committee
The use of CPT codes began over 50 years ago with the purpose of developing uniform language for coding medical services and procedures. This system was designed to standardize reporting practices and to increase the accuracy and efficiency in coding and billing. CPT codes are also used for administrative management purposes, claims processing, guideline development, and performance metrics (AMA, 2021). All CPT codes must be linked to appropriate International Classification of Diseases (ICD) codes.
New CPT codes are developed through a multitiered committee system, including the American Medical Associations (AMA) CPT Editorial Panel and affiliated Advisory Panels. This process can take many years, as seen for endoscopic, endonasal, transsphenoidal excision of pituitary adenomas (CPT 62165), which was implemented in 2003, nine years after codes for open resection were approved (Pollock, 2019).
When a new CPT code is formally adopted, it is assigned a relative value unit (RVU) by the Centers for Medicare & Medicaid Services (CMS). RVUs are numerical values that represent the cumulative value of physician labor, material expenses, institutional resources, and nonclinical resources required to perform that procedure. The related work-RVU (wRVU) more closely tracks technical, physical, and logistical costs incurred by individual providers. Both RVU and wRVU can be used by institutions and departments to determine surgeon productivity and salary.
Problems with the correct application of CPT codes often occur in three settings. In the most commonly encountered scenario, new innovations in patient care and technology can lead to treatments without a CPT code assignment.
The second setting leading to confusion is coding for procedures involving two or more surgeons with different specialty or subspecialty training. At adoption, each CPT code has been assigned a co-surgeon indicator level:
- 0 (co-surgeon not permitted)
- 1 (co-surgeon allowed with appropriate documentation)
- 2 (co-surgeon permitted without additional documentation).
Co-surgical cases are indicated by a -62 modifier. Reimbursement of -62 modified codes is set at 125% of the RVU value, which is divided equally between the co-surgeons.
Finally, coding issues can arise when older CPT codes are not deleted by CMS and the CPT Editorial Panel after newer CPT codes are established for a procedure, leading to multiple codes for the same procedure. Without clear guidance from CMS and the CPT Advisors, coding can become arbitrary, based on historical, geographic, or system-based preferences. Also, given the lack of regulator clarity, third- party consultancy organizations have submitted opinion-based recommendations that are often interpreted, inappropriately, as official guidelines.
Following the inaugural institution of CPT codes in the 1960s, the so-called Traditional or Legacy codes were developed for removal of vestibular schwannomas. These codes encompassed both the approach (type of craniotomy) and resection of the tumor within a single code (Table 1). As an example, a retrosigmoid craniotomy with excision of tumor would be coded as CPT 61520.
Table 1. Traditional CPT Codes for Vestibular Schwannoma (VS) Excision1
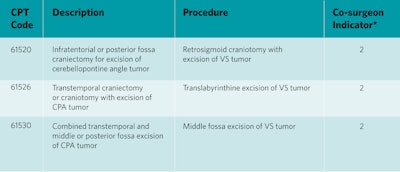 1Derived from AMA, 1993.
1Derived from AMA, 1993.
Abbreviations: CPA, cerebellopontine angle; CPT, Current Procedural Terminology
*Co-surgeon indicator: 0 = co-surgeon not permitted; 1 = co-surgeon may be allowed if documentation supports; 2 = co-surgeon permitted without additional documentation.
For vestibular schwannoma resection, these codes are linked to ICD10 code D33.3, benign neoplasm of the cranial nerves.
Prior to the 1900s, most lateral skull base procedures were performed exclusively by neurosurgeons. Pioneering efforts to demonstrate the safety and efficacy of the translabyrinthine and middle fossa approaches for excision of vestibular schwannomas led to increasing co-surgical treatment paradigms involving otolaryngologists and neurosurgeons.
Over time however, Traditional CPT codes were found to be lacking by many skull base surgeons in their ability to capture variations in case-complexity and operative time/effort associated with vestibular schwannoma resection. This issue was exacerbated by improvements in operative technology and preoperative imaging (allowing earlier detection of tumors). Additionally, surgery was progressively applied to a wider variety of tumor presentations. By 1990, most neurosurgical and neurotologic skull base surgeons agreed that the Traditional CPT codes representing surgical management of these highly variable procedures were insufficient.
In the early 1990s, a prominent panel comprised of a neurotologist (John Leonetti, MD) and two neurosurgeons (Thomas Origitano, MD, PhD, and Byron Pevehouse, MD) was tasked by the North American Skull Base Society with developing a new set of open lateral Skull Base CPT codes. The panel began by officially determining there were no existing codes that adequately described the procedures and division of labor associated with such cases in the modern era. Over the course of many years, the panel described and generated new codes to allow for more accurate coding of lateral skull base procedures.
The panel generated a list of 98 novel CPT codes designed to cover a variety of skull base tumor surgeries, including surgery for the average size vestibular schwannoma. The panel also determined the surgical approach should be coded separately from the surgical resection of the tumor. This list was ultimately reduced by CMS to the currently adopted 28 CPT codes, which include “Approach” and paired “Resection” codes (also known as “Skull Base” codes; Table 2). If an Approach code is performed and billed, then a corresponding Resection code should also be billed, either by the same surgeon if working alone or a different surgeon in a co-surgical setting.
Table 2. Paired Approach/Resection CPT Codes for Vestibular Schwannoma (VS) Excision2
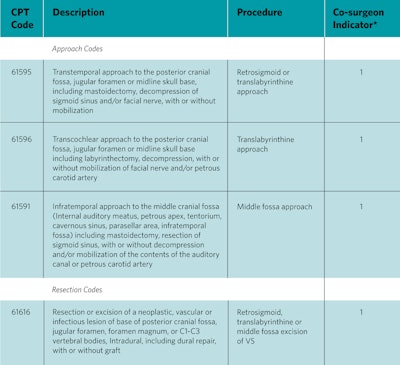 2Derived from AMA, 1993.
2Derived from AMA, 1993.
Abbreviations: CPT, Current Procedural Terminology; VS, vestibular schwannoma
*Co-surgeon indicator: 0 = co-surgeon not permitted; 1 = co-surgeon may be allowed if documentation supports; 2 = co-surgeon permitted without additional documentation.
For vestibular schwannoma resection, these codes are linked to ICD10 code D33.3, benign neoplasm of the cranial nerves.
Compared to the “Traditional” coding example mentioned previously, a retrosigmoid craniotomy with excision of tumor would be coded using the paired Approach and Resection codes with CPT 61595 and 61616 and linked to ICD code D33.3. Using these codes, co-surgeons can choose to take credit for either the Approach or the Resection code. Alternatively, the co-surgeons could be credited for both CPT codes and apply the -62 modifier. These Approach/Resection codes have a co-surgeon indicator score of 1, which requires additional documentation to specify why co-surgeons were needed for that code. This documentation requirement can lead to increased insurance denials and extra effort and time from coding experts to resubmit claims. Such issues are one of the reasons professional coding groups and insurance companies have advocated for use of the singular Traditional CPT codes (co-surgeon indicator 2 – no additional documentation required) over the paired Approach/Resection CPT coding.
Ideally, older (or possibly obsolete) CPT codes would have been deleted as newer codes are described and accepted. In the case of vestibular schwannoma surgery, this has not been the case. At this time, the AMA CPT Editorial Panel and CMS formally recognize both the Traditional and paired Approach/Resection CPT coding schemes.
Not surprisingly, there is a lack of consensus on how to apply these codes. Despite formal acceptance by CMS of the paired Approach/Resection codes in 1994, many surgeons have continued to use the Traditional codes. A survey of the American College of Surgeons National Surgical Quality Improvement Program data (ACS-NSQIP) published in 2019 reported that 75.6% of the reported lateral skull base codes used from 2010 to 2014 were Traditional codes, with the remaining 23.4% using paired Approach/Resection codes (Bi, 2019). Within this same study, coding of the same lateral skull base surgeries performed for excision of vestibular schwannoma from two high volume institutions (Brigham and Women’s Hospital 2005 and 2017 and the Barrow Neurological Institute between 2013 and 2017) were retrospectively reviewed for histopathologic confirmation of diagnosis, operative approach, surgeon affiliation (neurosurgery, neurotology, or both), and CPT code.
Perhaps to resolve the issues over proper coding practice, professional societies and third-party institutions have begun efforts at publishing coding tips and action statements to guide their membership and clientele. One such example includes coding tips from the American Association of Neurologic Surgeons (AANS), which state that the Skull Base codes should not be used in cases of cerebellopontine angle tumors because the “skull base approach is already included in the 61526 and 61520 codes” (Kimmel, 2022). Further, the 2022 AANS Guide to Coding does not include paired Approach/Resection codes in the treatment of cerebellopontine angle (CPA) tumors, despite the involvement of two prominent neurosurgeons and the North American Skull Base Society (NASBS) in creating those codes (Cheung, et al., 2022). After careful examination, this recommendation to exclude use of the paired Approach/Resection CPT codes appears to have been based on a single, third-party, editorial/opinion publication.
This letter recommended exclusive use of Traditional CPT codes for vestibular schwannomas due to the belief that the Approach/Resection code set was developed for “operating on a portion of the skull which was inaccessible prior to the development of innovative surgical approaches to lesions affecting the deep facial structures that are adjacent to the undersurface of the cranium.” The author of this opinion felt that vestibular schwannoma surgery did not meet this innovation requirement given surgery for these tumors existed prior to 1990 (Pollock, 2019).
Ultimately, the plurality of codes available for lateral skull base surgery will need to be to be addressed at some point. The confusion and controversy surrounding proper application of the codes has led to multiple, unsustainable problems for professionals. Chief among these, as previously mentioned, is in the domain of insurance billing and collections. Additionally, conflicts between coders, neurosurgeons, and neurotologists are common and lead to unnecessary friction between otherwise cohesive clinical teams. Thirdly, academic and administrative use of CPT codes for research and practical purposes may be heavily disrupted by a plural coding system. This can lead to inaccurate representation of skull base surgical productivity, potentially harm provider compensation, and possibly lead to incomplete clinical/outcomes data reporting.
Finally, resident and fellow education on proper coding is harmed by a plural coding situation. Graduates entering practice may have been taught codes that do not comply with their new institution’s norms, leading to potential conflict. Additionally, ACGME requirements regarding neuro-otology fellowship case logs includes a mixture of Traditional and paired Approach/Resection codes that will likely not conform to future professional coding expectations they will encounter after graduation.
To date, the AMA CPT Editorial Panel, CPT Advisory Panels, and CMS have not published official guidelines to clarify coding for vestibular schwannoma resection. At this time, both the Traditional and Skull Base coding sets may be applied to surgical treatment of vestibular schwannomas. Neurotologists and neurosurgeons are encouraged to investigate this situation with their coders and institutions.
Acknowledgment: We thank Natalie Workman, CPC, Indiana University, for review of this article and assistance with editing.
References
American Medical Association (AMA) “CPT overview and code approval.” https://www.ama-assn.org/practice-management/cpt/cpt-overview-and-code-approval, accessed 6/21/2023.
American Medical Association (AMA). “Coding Clarification: Skull Base Surgery,” CPT Assistant Winter 1993: 15 – 19.
Cheung JS, Ratcliff JK, Tumarkin LM. 2022 AANS Guide to Coding: Mastering the Global Service Package for Neurological Surgery Services, American Association of Neurological Surgeons (AANS), 2021.
Bi WL, Mooney MA, Yoon S, Gupta S, Lawton MT, Almefty KK, Corrales CE, Dunn IF. “Variation in coding practices for vestibular schwannoma surgery,” J Neurol Surg B 2019: 80(1);96-102.
Kimmell K. “AANS Coding Short: Cerebellopontine Angle Tumor Resection,” https://vimeo.com/553494754/6da9dcb4ae?embedded=true&source=vimeo_l ogo&owner=22709940.
Leonetti JP, Shohet JA, Buckholtz R. “Ensuring proper reimbursement in the Affordable Care Act Environment: Acceptable coding strategies and practice tips for neurotologists,” American Neurotology Society Fall Meeting, Dallas Texas, 2015.
Pollock K. “Variation in coding practice for vestibular schwannoma surgery,” J Neurol Surgery B 2019:80(1);103-104.
Pollak KJ, the NASBS Best Practices for Coding & Billing Task Force: Casiano RR, Folbe AJ, Golfinos JG, Snyderman CH. “Coding and reimbursement for endoscopic endonasal surgery of the skull base,” J Neurol Surg B Skull Base 2019:80(Suppl 2);S247-254.