Physician safety is patient safety: Good surgical ergonomics to optimize patient care
Physicians selflessly provide care to their patients over the course of a 30 to 40-year career. Ideally, we stay healthy and rarely get sick or suffer a serious injury. However, we are not immune from physical infirmity and—like a professional athlete—simply often choose to “play through the pain.”
Daniel L. Wohl, MD and Theresa Hubbard, DPT for the PSQI Committee
Physicians selflessly provide care to their patients over the course of a 30 to 40-year career. Ideally, we stay healthy and rarely get sick or suffer a serious injury. However, we are not immune from physical infirmity and—like a professional athlete—simply often choose to “play through the pain.” We function in a stressful environment and need to be mindful of how the physical demands of our stressful profession impact our ability to provide optimal care for our patients. Establishing and maintaining consistent proper physical ergonomic movements and body positioning is required to avoid developing career-limiting physical ailments. The practice of otolaryngology-head and neck surgery requires us to repetitively position our bodies to obtain optimal visual and physical access when examining and operating upon patients. This translates to numerous instances where we might lean and strain the lower back, overly hang our heads on flexed necks, or twist something just a bit more, and wind up struggling and sore.1, 2, 3, 4, 5
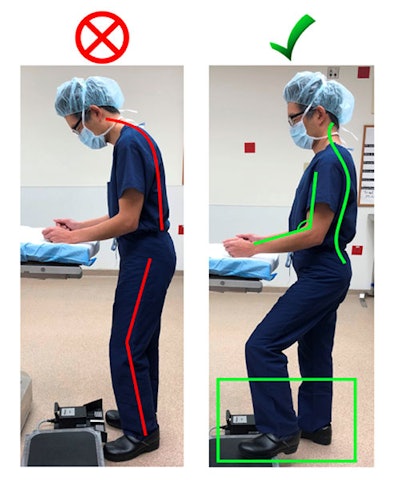 Figure 1. Left: Bad posture lateral view: Line shows forward head and leaning posture throughout spine. Neck is flexed more than 45 degrees. Right: Good posture lateral view. Line shows more neutral spine curves and good elbow joint angle (90-120 degrees). Symmetrical stance with one foot placed on foot stool.
Figure 1. Left: Bad posture lateral view: Line shows forward head and leaning posture throughout spine. Neck is flexed more than 45 degrees. Right: Good posture lateral view. Line shows more neutral spine curves and good elbow joint angle (90-120 degrees). Symmetrical stance with one foot placed on foot stool.During a long surgical case, it is easy to display poor posture, commonly with forward head and shoulders with excessive leaning and hunched back (Figure 1). Postural impairments like these often lead to musculoskeletal complaints. Good posture involves maintaining the natural curvatures of the spine: an inward curve in the low back and neck joined by an outward curve in the thoracic spine. Adjusting table height is one way to avoid poor posture and maintain these natural curves. The table should be at a height where the top of the patient is at waist level to the surgical team. We are all different shapes and sizes, so individuals should sit, stand, or stand on a platform in order to achieve correct positioning next to the table. If using video monitors, eyes should be in line with the top edge of the monitor, allowing 15-20 degrees of flexion when looking at the center of the screen.6
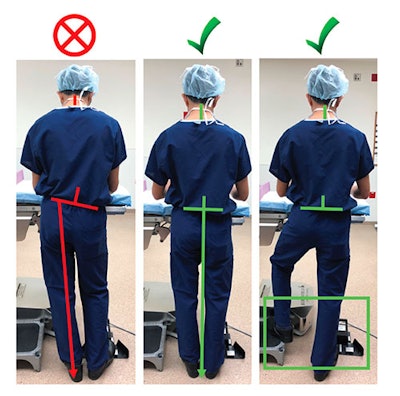 Figure 2. Left: Bad posture posterior view: asymmetrical weight bearing is evident by tilted pelvic line and non-vertical alignment of lumbar spine. Middle: Good posture without step stool. Lines demonstrate neutral lumbar and pelvic alignment. Right: Good posture with step stool.
Figure 2. Left: Bad posture posterior view: asymmetrical weight bearing is evident by tilted pelvic line and non-vertical alignment of lumbar spine. Middle: Good posture without step stool. Lines demonstrate neutral lumbar and pelvic alignment. Right: Good posture with step stool.With consideration to the lower body, weight should be evenly distributed through both legs (Figure 2). Prolonged shifting of weight to one leg leads to an asymmetrical stance and increases strain on the pelvis and lumbar spine. Instead, rest one foot on a small step stool to decrease pressure and fatigue in the back and legs without assuming an asymmetrical position. Foot pedal position can lead to an asymmetrical stance if not considered carefully. Foot pedals should be placed near the foot and aligned in the same direction as instruments and toward the target quadrant of the patient. If standing on a platform, the foot pedal should also be on the platform. Foot pedals with built-in foot rests are more ergonomic because the foot isn’t moving back and forth as frequently or being actively held above the pedal when it is not in use. Varying which foot uses the pedal throughout cases will help decrease muscle imbalances that occur with repetitive movements.
 Figure 3. Top: Microscope height placed too low and with downward angled eyepieces, requires the surgeon to flex the neck. Bottom: Eyepiecesoriented with only slight declination allows the surgeon to operate with the head in a more upright neutral neck position.
Figure 3. Top: Microscope height placed too low and with downward angled eyepieces, requires the surgeon to flex the neck. Bottom: Eyepiecesoriented with only slight declination allows the surgeon to operate with the head in a more upright neutral neck position.Switching to a seated position and readjusting the table height also alleviates fatigue from standing. While seated, hips and knees should both be flexed to 90 degrees. Feet should be placed on the floor or a platform to prevent legs from dangling unsupported. Use of an adjustable chair with articulated arm supports decreases neck strain and shoulder torque when performing laryngeal surgery. Arm rests help resist the tendency of upward shoulder migration. Arm rest height should be adjusted to allow for a 90-120-degree elbow joint angle when shoulders are relaxed. Proper microscope positioning is required to preserve cervical spine ergonomics (Figure 3).
Prolonged excessive downward neck flexion with arms forward develops long and weak stabilizing musculature in the cervical spine and scapular region. This weakness correlates with overuse of pectorals, upper trapezius, and levator scapulae. Exercises that emphasize posterior tilt and retraction of the scapulae with retraction of the cervical spine will help strengthen and retrain weak muscles to overcome overused muscles. Training will help counteract and correct muscle imbalances, leading to less risk of injury. “Microbreak” exercises can also be performed throughout the day to counteract prolonged positioning.8
The successful professional athlete knows that bad habits are hard to unlearn. The key is to develop good habits early. It is the same with surgeons. Our success is reliant on skilled physical movements, maintenance of focus, and the ability to make necessary adjustments as the situation requires. Good ergonomics takes practice and experience. We are no less vulnerable to physical and mental fatigue, over any one game, over a long season, and especially over a long productive career. Popular culture says that it takes 10,000 times to get really good at something. Over the course of your career, you will perform at least one procedure 10,000 times. You might as well do it with good physical ergonomics.
References:
1 Bolduc-Bégin J, François Prince ·, Christopoulos A, Tareck Ayad ·. Work-related musculoskeletal symptoms amongst Otolaryngologists and Head and Neck surgeons in Canada. Eur Arch Otorhinolaryngol. 2018;275:261-267.
2 Vaisbuch Y, Aaron KA, Moore JM, Vaughan J, Ma Y, Gupta R, Jackler RK. Ergonomic hazards in otolaryngology. Laryngoscope. 2019 Feb;129(2):370-376
3 Ho TT, Hamill CS, Sykes KJ, Kraft SM. Work-related musculoskeletal symptoms among otolaryngologists by subspecialty: A national survey. Laryngoscope. 2018;128(3):632-640.
4 Cavanagh J, Brake M, Kearns D, Hong P. Work environment discomfort and injury: an ergonomic survey study of the American Society of Pediatric Otolaryngology members. Am J Otolaryngol. 2012 Jul-Aug;33(4):441-6.
5 Wong A, Baker N, Smith L, Rosen CA. Prevalence and risk factors for musculoskeletal problems associated with microlaryngeal surgery: A national survey. Laryngoscope. 2014;124(8):1854-1861.
6 Ramakrishnan VR, Montero PN. Ergonomic considerations in endoscopic sinus surgery: Lessons learned from laparoscopic surgeons. Am J Rhinol Allergy. 2013;27:245-250.
7 Statham MMC, Sukits AL, Redfern MS, Smith LJ, Sok JC, Rosen CA. Ergonomic analysis of microlaryngoscopy. Laryngoscope. 2010;120(2):297-305.
8 Hallbeck MS, Lowndes BR, Bingener J, Abdelrahman AM, Yu D, Bartley A, Park AE. The impact of intraoperative microbreaks with exercises on surgeons: A multi-center cohort study. Appl Ergon. 2017 Apr;60:334-341.



















