Developing a Tutorial for Breastfeeding Surgeons
Addressing the specific logistic challenges of breastfeeding as a practicing surgeon or trainee can help women remain in the field and thrive.
Carly Clark, MD, and Nikita Gupta, MD, on behalf of the Women in Otolaryngology Section


According to a survey conducted by Rangel et al. of general surgery residents who had one or more pregnancies during residency, respondents had striking responses about their work experiences with both pregnancy and breastfeeding. Of the participants, 39% seriously considered leaving residency and 30% reported they would advise women medical students against pursuing a career in surgery because of dissatisfaction with their pregnancy experience, maternity leave options, and inadequate lactation support.3
Breastfeeding is important to physician-mothers; research indicates that they initiate breastfeeding at above-average rates compared with the general population.3,4 Nevertheless, their busy schedules, unpredictable hours, and limited access to lactation rooms or breastfeeding equipment serve as significant barriers to meeting breastfeeding goals. Those in surgical fields report feeling less supported and encountering more work-related obstacles compared with those in non-surgical medical specialties. 5
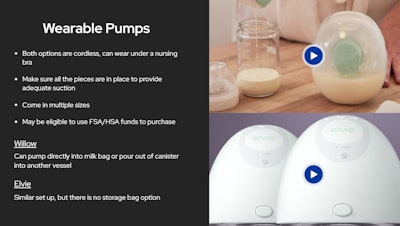
The module addresses issues including finding pumping locations, wearable pumps, pumping in the operating room or in between cases/clinic patients, breastmilk storage, hydration/caloric intake, finding time to pump or feed, considerations for call, as well as tips for success from those who have gone through the experience.
Otolaryngology is a unique specialty in which clinic plays a large role, including various procedures, as well as a range of very short operative procedures with quick turnover and multi-hour operative cases. Breastfeeding otolaryngologists are pulled in many directions during the workday, including for emergencies at a moment’s notice, such as blocked airways. Thus, they serve as a great target audience for our module. However, because we were unable to find similar resources for other specialties, we have broadened the scope of the module to include all breastfeeding surgeons.
Responses to the module have been overwhelmingly positive, including among non-surgeon breastfeeding physicians:
“Just wanted to say congrats and thank you. This was really well done and needed! I'm currently nine months into breastfeeding (both direct feeding and pumping) and echo many of the sentiments in the video. Although not navigating the OR, navigating a busy clinic in a surgical practice as the first female to take maternity leave as well as covering athletics events has had its fair share of challenges. It was comforting hearing I wasn't alone in my thoughts, frustrations and successes in those avenues. I hope this continues to gain momentum and [I am] happy to help in the future if needed to mentor others in their breastfeeding journey. Thanks again for normalizing motherhood in medicine!”
“As a breastfeeding mother in medicine, I am experiencing the challenges of finding adequate time to pump and eat/drink throughout the day. I cannot imagine how much harder it is as a surgeon. I am in awe of you. Thank you for this work. It has inspired me to advocate the same way for women neurologists.”
While our module is a good start, additional changes must be made to support surgeons’ breastfeeding goals, particularly during residency. Although ACGME requirements state that residency programs must provide “‘clean and private facilitates for lactation that have refrigeration capabilities, with proximity appropriate for safe patient care,"6 residents still report poor access to lactation facilities and challenges leaving the operating room to pump. 3
Some programs have developed innovative solutions for addressing these concerns by providing wearable pumps for residents to use while working or operating. For example, the Kansas University Graduate Medical Education office developed a program to provide wearable pumps and mini fridges for storing milk to residents on loan for up to one year. Feedback from this program suggests that these materials alleviated some of the barriers to breastfeeding, such as access to lactation rooms and improved clinical work productivity.7 Another program was developed at the University of Wisconsin to provide cross-coverage for lactating residents in the operating room.8 When lactating residents needed to express milk, an additional resident on the team would assist in the operating room during non-critical portions of the case until the lactating resident could return.
These programs were both developed in response to feedback from residents and highlight the importance of checking in with trainees to ensure they feel supported and have the resources required to succeed in their breastfeeding goals.

We hope that our resource helps new mothers but also raises awareness of the barriers to success that female surgeons so often quietly overcome. Following completion of the module, we aim to evaluate participant satisfaction and knowledge regarding breastfeeding to adjust the module as needed. We must continually engage surgeon-mothers in our field and acknowledge the challenges they face in navigating childbearing, breastfeeding, and taking care of patients.
References
- Mroz J. A Medical Career, at a Cost: Infertility. New York Times. September 13, 2021.
- Stentz, NC, Griffith KA, Perkins E, Jones RD, Jagsi R. Fertility and Childbearing Among American Female Physician. J Womens Health (Larchmt). 2016 Oct;25(10):1059-1065.
- Rangel EL, Smink DS, Castillo-Angeles M, et al. Pregnancy and Motherhood During Surgical Training. JAMA Surg. 2018;153(7):644-652. doi:10.1001/jamasurg.2018.0153
- Sattari M, Levine DM, Mramba LK, et al. Physician Mothers and Breastfeeding: A Cross-Sectional Survey. Breastfeed Med. 2020;15(5):312-320. doi:10.1089/bfm.2019.0193
- Sattari M, Levine D, Neal D, Serwint JR. Personal breastfeeding behavior of physician mothers is associated with their clinical breastfeeding advocacy. Breastfeed Med. 2013;8(1):31-37. doi:10.1089/bfm.2011.0148
- ACGME Common Program Requirements (Residency). Accreditation Council for Graduate Medical Education (ACGME). 2023; 6.
- McMillin A, Behravesh B, Byrne P, Unruh GK. A GME Wearable Breast Pump Program: An Innovative Method to Meet ACGME Requirements and Federal Law. J Grad Med Educ. 2021;13(3):422-423. doi:10.4300/JGME-D-20-01275.1
- Livingston-Rosanoff D, Shubeck SP, Kanters AE, Dossett LA, Minter RM, Wilke LG. Got Milk? Design and Implementation of a Lactation Support Program for Surgeons. Ann Surg. 2019 Jul;270(1):31-32. doi: 10.1097/SLA.0000000000003269. PMID: 30921050