Severe Tinnitus: A Brain Disorder Beyond the Ringing Sound
Severe tinnitus is a systemic brain condition requiring multimodal, rehabilitative care models to comprehensively address its complex nature.
Hamid R. Djalilian, MD*, and Mehdi Abouzari, MD, PhD, on behalf of the Hearing Committee

Strategies to treat tinnitus have historically suffered from a sound therapy-centric focus, viewing the condition as primarily an auditory phenomenon that needs to be masked. This perspective has hindered the development of effective interventions, particularly for severe or fluctuating tinnitus. Mild tinnitus and severe tinnitus are not merely points on a spectrum of loudness. Rather, severe tinnitus represents a fundamentally different condition, involving multiple brain regions and systemic dysfunctions far beyond the auditory system.
It is now evident that severe tinnitus is a complex multisystem brain disorder. Although its primary symptom is auditory, severe tinnitus shares significant similarities with central sensitization syndromes and atypical migraine. These conditions involve systemic dysregulation, heightened neural excitability, and neurogenic inflammation, which impact networks responsible for emotion, attention, and sensory processing. Recognizing this distinction is essential for developing effective treatments. This article reframes severe tinnitus as a systemic brain condition and advocates for a shift toward multimodal, rehabilitative care models to address its complex nature comprehensively.
The Failure of Sound Therapy-Centric Approaches
For decades, tinnitus has been framed as primarily a dysfunction in the auditory pathway, attributed to hyperactivity in the auditory brainstem resulting from hearing loss. Although this explanation accounts for some cases, it fails to address the broader clinical realities of severe tinnitus. Patients frequently report experiences that extend beyond auditory phenomena, such as “good days” with quieter tinnitus, and “bad days” when the tinnitus becomes overwhelmingly loud. Others describe sudden and unpredictable changes in tinnitus triggered by infections, vaccination, stress, hormonal fluctuations, or external stimuli.1 Many also report somatic tinnitus, where jaw, neck, or facial manipulations can modulate the sound.2
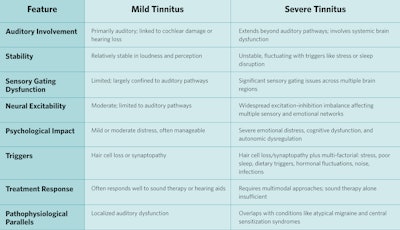
This instability in the tinnitus level underscores that severe tinnitus extends far beyond the auditory system, marking one of the many differences between mild and severe tinnitus (see Table 1). Central auditory hyperactivity is a necessary condition, but it is not sufficient to explain the entire severe tinnitus phenotype. Severe tinnitus arises when broader dysfunctions in the brain map onto this auditory hyperactivity, amplifying it into a problem involving multiple different brain networks.3 Neuroinflammation, imbalances between neural excitation and inhibition, and central sensitization drive this process, transforming a localized auditory issue into a complex multisystem disorder.4
Table 1: Key distinctions between mild and severe tinnitus.
Sound-centered interventions, such as masking therapies and hearing aids, are not well-equipped to address these neurobiological features of severe tinnitus.5 They are incapable of targeting the underlying neurogenic inflammatory processes, excitation-inhibition imbalances, and systemic dysfunctions that characterize severe tinnitus. Consequently, they frequently leave patients with inadequate relief and perpetuate the misconception among clinicians that “nothing can be done” for tinnitus.
This inadequacy has fueled a harmful ecosystem of pseudoscientific remedies, including herbal supplements and “miracle cures,” which exploit the desperation of tinnitus sufferers. These unproven interventions highlight the urgent need for a paradigm shift in how tinnitus is understood and treated. Effective care must address the neurobiological underpinnings of severe tinnitus, creating a foundation for multimodal treatment strategies to deliver meaningful relief.
Severe Tinnitus as Atypical Migraine
Migraine is increasingly being redefined as a disorder of sensory processing and sensory gating, where the brain struggles to regulate and prioritize sensory inputs.6 This sensory dysregulation is now understood to be at the core of migraine, manifesting in hypersensitivity to light, sound, and other environmental stimuli. Central to this revolutionary concept is the recognition that the migraine reaction is fundamentally neuroinflammatory in nature.7 The discovery of the role of calcitonin gene-related peptide (CGRP)—a neuropeptide involved in the transmission of pain and inflammation—has been transformative in understanding migraine. CGRP not only drives the neuroinflammatory cascade but also amplifies sensory hypersensitivity, making even mild stimuli feel overwhelming.8 These insights into the neuroinflammatory underpinnings of migraine have shed light on its connection to severe tinnitus.
Severe tinnitus shares this threshold-dependent mechanism with migraine, where minor changes in neuroinflammatory factors can precipitate a major symptomatic event.9 Stress, poor sleep, dietary triggers, certain stimulations (e.g., sound or atmospheric pressure changes), and even hormonal shifts act as additive factors, incrementally increasing neuroinflammation. Once the cumulative burden exceeds the individual’s threshold for neural stability, this can result in an episode of loud, intrusive tinnitus. This concept of a threshold disease explains why severe tinnitus, much like migraine, is often unpredictable and episodic, with fluctuations in severity tied to environmental and internal stressors.10
Both conditions exhibit dysregulated sensory networks, particularly involving the salience network and thalamocortical circuits.11 In both conditions, this dysregulation leads to neuronal hyperactivity which disrupts sensory processing and amplifies sensitivity. Both conditions also manifest thalamocortical dysrhythmia, where aberrant brain rhythms contribute to the amplified perception of phantom sounds.12 These shared neurological phenomena underscore the systemic nature of both disorders, moving beyond the localized symptoms of headache or ringing to implicate global brain dysfunction.
The episodic nature of severe tinnitus further aligns with migraine as a threshold disease. During periods of low neuroinflammatory activity, the brain maintains its ability to suppress or filter out irrelevant sensory inputs, keeping tinnitus quieter and less intrusive. However, when cumulative triggers such as disrupted sleep, heightened stress, overstimulation, hormonal fluctuations, or dietary factors increase neuroinflammation, this balance is lost, and tinnitus flares. This dynamic interplay between neuroinflammation, sensory processing, and environmental factors reinforces the conceptual link between migraine and severe tinnitus, framing both as disorders of sensory overload and central nervous system sensitization.
Recognizing severe tinnitus as a sensory gating disorder similar to atypical migraine not only advances our understanding of its pathophysiology but also opens new avenues for treatment. By balancing neurotransmitters, targeting neuroinflammatory pathways, and addressing lifestyle factors that contribute to the migraine process, we can raise the threshold for tinnitus exacerbations, offering patients more stability and control over their symptoms. This evolving perspective underscores the need for an integrated, multidisciplinary approach to managing severe tinnitus within the broader framework of brain sensitivity disorders.
Central Sensitization and Tinnitus
Central sensitization (CS) refers to a state in which the central nervous system (CNS) becomes hyper-responsive to stimuli, amplifying sensory input and generating symptoms even in the absence of external triggers.13 Initially described in the context of chronic pain, CS has since been recognized as a unifying mechanism underlying a range of chronic sensory hypersensitivity conditions, such as fibromyalgia, irritable bowel syndrome, and migraine. Emerging evidence suggests that severe tinnitus, like these conditions, follows a similar trajectory of sensory dysregulation and heightened neural sensitivity.14
The model of central sensitization builds on the foundational neurophysiological framework introduced by Jastreboff, who described tinnitus as arising from aberrant auditory activity amplified and perpetuated by emotional and attentional networks in the brain.15 Over time, this concept has been refined to integrate insights from pain neuroscience and sensory processing research. CS reframes tinnitus as not merely an auditory phenomenon but part of a broader dysfunction in sensory gating and regulation, where the CNS amplifies internal signals, such as spontaneous activity in the auditory system, while failing to filter irrelevant inputs.
Neuroimaging studies of severe tinnitus reveal patterns of brain activity that align closely with CS-related conditions.16 Aberrant activation has been identified in regions responsible for sensory processing, emotion regulation, and attention, including the anterior cingulate cortex, insula, and amygdala. These areas are part of the salience network, which prioritizes sensory signals for conscious processing. The salience center decides what is important and deserves more attention. In severe tinnitus, the salience network becomes dysregulated, amplifying the perception of tinnitus and assigning it undue significance.16 This parallels the mechanisms of CS in conditions like fibromyalgia and migraine, where sensory inputs are similarly overprocessed, leading to exaggerated and persistent symptoms.
At the neurochemical level, severe tinnitus and other CS-related disorders share common pathways, particularly involving the brain’s primary excitatory and inhibitory neurotransmitters.17 This imbalance underpins the heightened neural excitability and reduced inhibitory control that are characteristic of both conditions. Calcitonin gene-related peptide (CGRP), a neuropeptide central to migraine pathology, also plays a significant role in CS and has been implicated in the neuroinflammatory processes underlying severe tinnitus.18 CGRP amplifies sensory hypersensitivity and perpetuates neural hyperactivity, creating a feedback loop that sustains central sensitization.
This new understanding of tinnitus as a manifestation of CS represents an evolution of Jastreboff’s original neurophysiological model. Although Jastreboff emphasized the auditory system’s interaction with limbic and attentional networks, the CS framework expands this to include systemic neuroinflammatory processes, dysregulated sensory gating, and maladaptive plasticity across the CNS. For example, oxidative stress and neuroinflammation—hallmarks of CS—exacerbate the excitation-inhibition imbalance in tinnitus, leading to a persistent state of sensory hyper-responsiveness. This aligns with findings in migraine and chronic pain, further supporting the shared underpinnings of these conditions.19
Importantly, CS does not occur in isolation but reflects a dynamic interplay between environmental, biological, and psychological factors. Stress, poor sleep, dietary triggers, sensory overstimulation, and hormonal fluctuations all contribute to the neuroinflammatory state that drives CS, lowering the brain’s threshold for sensory overload.20 This threshold model explains the episodic nature of severe tinnitus, where seemingly minor stressors can push the CNS into a heightened sensitization state, resulting in louder, more intrusive tinnitus. Understanding tinnitus through the lens of central sensitization provides a comprehensive framework for addressing its underlying mechanisms, offering a pathway toward more effective, multimodal treatment strategies.
The Role of Pharmacology in Stabilizing Severe Tinnitus
Pharmacological interventions are essential for managing the instability and intensity of central sensitization and thus severe tinnitus. These treatments aim to stabilize neural circuits, reduce neuroinflammation, and balance excitation and inhibition, creating the necessary conditions for other therapeutic modalities to succeed. Severe tinnitus, marked by its cyclic flare-ups and unpredictability, involves a cascade of limbic system arousal, sensory network hyperactivity, and central sensitization. Medications tailored to interrupt these cycles serve as a vital bridge to long-term rehabilitative care.21
Pharmacological approaches targeting migraine-like neural pathways are particularly promising. Anti-seizure medications, for instance, help prevent cortical spreading depression, a phenomenon observed in migraine and hypothesized to play a role in central sensitization and thus tinnitus exacerbations. Medications can restore the excitation-inhibition balance critical for stabilizing the auditory system. Recent studies combining antidepressants with antiseizure medications or calcium channel blockers have shown significant reductions in tinnitus-related distress, further highlighting the potential of pharmacological synergy.22
Neuroinflammatory pathways are also critical targets. Anti-inflammatory agents, such as vitamins and supplements, may reduce the neurogenic inflammation that perpetuates central sensitization and tinnitus intensity.23 Migraine-specific drugs that act on CGRP pathways may reduce neuroinflammatory cascades and hyper-responsiveness in sensory networks. While still under investigation, these interventions may address tinnitus loudness at a systemic level, targeting its biological roots rather than its symptoms alone.
Pharmacology, however, should not be viewed as a standalone solution. Rather, it serves as a foundation for stabilizing the brain’s neural environment, enabling traditional interventions, such as sound therapy, cognitive behavioral therapy (CBT), mindfulness, and neuroplasticity-based approaches, to gain traction. By reducing the intensity and unpredictability of tinnitus, pharmacological stabilization enhances the efficacy of these therapies, facilitating long-term improvements in symptom management and overall quality of life.
Multimodal Treatment: Addressing the Whole Patient
Given the systemic and multifactorial nature of severe tinnitus, a multimodal approach to treatment is essential. This strategy integrates medical, psychological, and lifestyle interventions to address the condition’s biological, cognitive, and emotional dimensions. While sound therapy plays a valuable role within this framework, it is ancillary rather than primary. The cornerstone of effective treatment lies in addressing neuroinflammation, central sensitization, and neurotransmitter imbalances that drive the condition.
Pharmacological interventions remain foundational for stabilizing severe tinnitus. These treatments aim to modulate neural excitability and restore the brain’s balance between excitation and inhibition.22 Anti-inflammatory and antioxidant therapies further mitigate the neuroinflammatory cascades that perpetuate neural dysregulation, enhancing the efficacy of pharmacological interventions. Personalized medication regimens provide a tailored approach, ensuring maximum therapeutic impact while addressing individual variability.
Lifestyle interventions are equally critical, acting as both preventative and therapeutic measures. By addressing the root causes of neuroinflammation and factors predisposing the brain toward excitation-inhibition imbalance, lifestyle modifications reduce the likelihood of reaching the threshold that triggers severe tinnitus. Poor sleep, chronic stress, and inflammatory dietary habits are key contributors to this imbalance, exacerbating neural hyperactivity and sensory hypersensitivity. Interventions targeting these factors, such as stress reduction, improved sleep hygiene, and dietary adjustments, help stabilize the brain’s sensory networks. For example, sleep hygiene and the treatment of sleep disorders restore the brain’s glymphatic system, which is essential for clearing inflammatory byproducts, while a targeted migraine diet prevents activation of the CS process. In this way, lifestyle medicine not only complements pharmacological treatments but also addresses the upstream factors driving dysregulation.
Behavioral therapies, such as cognitive-behavioral therapy (CBT), acceptance and commitment therapy (ACT), and mindfulness-based interventions, are critical for reducing the cognitive and emotional burden of tinnitus.24 These approaches equip patients with tools to reframe distressing thought patterns, decrease hypervigilance, and build resilience against flare-ups. CBT, in particular, has demonstrated efficacy in breaking the cycle of anxiety and amplification that worsens tinnitus perception. Practices like yoga, meditation, and deep breathing exercises further enhance autonomic regulation, reducing physiological stress, promoting neural recovery, and lowering the overall inflammatory burden.
In combination, these interventions form a cohesive treatment plan. Pharmacology raises the brain’s threshold for triggering tinnitus, while lifestyle modifications reduce the factors that predispose the brain to instability (see Figure 1). Together, they provide a comprehensive approach to managing severe tinnitus, targeting its root causes and promoting long-term stability and recovery.
 Figure 1. Tinnitus follows atypical migraine pattern.
Figure 1. Tinnitus follows atypical migraine pattern.
Severe tinnitus exhibits a pattern resembling atypical migraine, characterized by fluctuating cortical activity influenced by neuroinflammatory triggers such as stress, poor sleep, and certain dietary factors. When these cumulative factors push cortical activity beyond the migraine threshold, there is an increase in central sensitization and more attention to the tinnitus percept, making it loud, intrusive, and disruptive, similar to the ictal phase of a migraine. Pharmacological interventions can raise this threshold, while comprehensive medical management helps stabilize the system, keeping symptoms below the critical threshold. This shift transforms tinnitus from an unstable to a stable state, creating the conditions necessary for habituation strategies to succeed—an outcome that is often unattainable in the context of fluctuating or severe tinnitus.
The Rehabilitation Model: A Path Forward
Effectively treating severe tinnitus requires more than a series of discrete interventions; it necessitates a comprehensive rehabilitation model of care. Severe tinnitus, like other conditions driven by central sensitization syndromes (CSS) or atypical migraine, is chronic and multifaceted, demanding an approach that prioritizes brain health through sustained, individualized support. This model acknowledges the interconnected roles of medical, psychological, and lifestyle factors while addressing the inherent challenges of functional medicine-based interventions.
One of the greatest barriers to success in treating conditions reliant on lifestyle modifications, such as severe tinnitus, is the lack of ongoing support. Without a structured framework, patients often struggle to make and sustain meaningful changes to stress management, sleep hygiene, diet, and physical activity—factors that are foundational to reducing neurogenic inflammation and restoring excitation-inhibition balance in the brain. The rehabilitation model directly addresses this limitation, providing the resources, guidance, and accountability needed to translate therapeutic recommendations into lasting behavioral change.
The primary goal of this approach is to promote overall brain health, recognizing that improving neural stability can resolve the central drivers of severe tinnitus. By stabilizing the underlying atypical migraine and CS processes, the rehabilitation model offers a pathway to long-term relief. Patients are empowered with education and tools tailored to their specific needs, enabling them to understand the condition and actively participate in their care. This sense of agency is critical for maintaining the lifestyle changes necessary to prevent flare-ups and reduce symptom severity over time.
Importantly, the rehabilitation model positions severe tinnitus as fundamentally similar to other CSS conditions, such as fibromyalgia, irritable bowel syndrome, and chronic fatigue syndrome (see Table 2). In all these cases, success depends on addressing the systemic dysfunctions that perpetuate neural hypersensitivity. Rehabilitation programs accomplish this by integrating medical management, such as pharmacological stabilization and anti-inflammatory therapies, with structured lifestyle interventions, including stress reduction techniques, sleep optimization, and dietary modifications. The result is a holistic, interdisciplinary framework that addresses the root causes of the condition rather than merely managing symptoms.
Table 2: Components of the rehabilitation model for severe tinnitus.
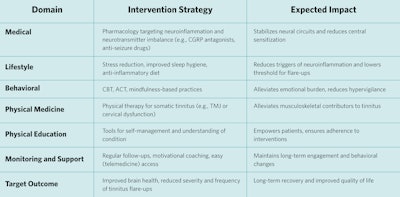
By prioritizing sustained support, patient education, and a systemic approach to care, the rehabilitation model provides a superior pathway for addressing severe tinnitus and similar conditions. This paradigm shifts the focus from symptomatic relief to long-term recovery, empowering patients to achieve meaningful improvements in their quality of life (e.g., improved sleep and reduced stress) while fundamentally improving their tinnitus.
Conclusion
Severe tinnitus is not just a ringing sound in the ears; it is a systemic brain disorder that shares significant similarities with CSS and atypical migraine. Recognizing this broader context is essential for developing effective treatments and overcoming the failures of sound-centric approaches. By adopting a multimodal, rehabilitation-based model of care, we can address the complex neurobiological, psychological, and lifestyle factors that drive severe tinnitus. Pharmacology serves as a critical stabilizing bridge, allowing traditional treatments to take effect and enabling long-term improvements. This holistic approach not only offers hope for patients but also represents a critical step forward in reimagining tinnitus as a treatable medical condition.
Author Disclosures:
Dr. Djalilian holds equity in Elinava Technologies, Cactus Medical LLC, and is an advisor and holds equity in NeuroMed Clinic, LLC. He holds patents on methods to treat tinnitus using electric stimulation of the cochlea and a medication combination.
References
- Lee A, Abouzari M, Akbarpour M, Risbud A, Lin HW, Djalilian HR, “A proposed association between subjective nonpulsatile tinnitus and migraine,” World J. Otorhinolaryngol. - Head Neck Surg., vol. 9, no. 2, pp. 107–114, Oct. 2022, doi: 10.1002/wjo2.8.1
- Michiels S, et al., “Conservative therapy for the treatment of patients with somatic tinnitus attributed to temporomandibular dysfunction: study protocol of a randomised controlled trial,” Trials, vol. 19, p. 554, Oct. 2018, doi: 10.1186/s13063-018-2903-.1
- Ridder DD, Vanneste S, Song SS, Adhia D, “Tinnitus and the Triple Network Model: A Perspective,” Clin. Exp. Otorhinolaryngol., vol. 15, no. 3, p. 205, Jul. 2022, doi: 10.21053/ceo.2022.00815.
- O’Hare L, Tarasi L, Asher JM, Hibbard PB, Romei V, “Excitation-Inhibition Imbalance in Migraine: From Neurotransmitters to Brain Oscillations,” Int. J. Mol. Sci., vol. 24, no. 12, p. 10093, Jun. 2023, doi: 10.3390/ijms241210093.
- “Cochrane corner: Sound therapy (using amplification devices and/or sound generators) for tinnitus - PubMed.” Accessed: Jan. 19, 2025. Online. Available: https://pubmed.ncbi.nlm.nih.gov/31361173/
- Goadsby PJ, Holland PR, Martins-Oliveira M, Hoffmann J, Schankin C, Akerman S, “Pathophysiology of Migraine: A Disorder of Sensory Processing,” Physiol. Rev., vol. 97, no. 2, pp. 553–622, Apr. 2017, doi: 10.1152/physrev.00034.2015.
- Biscetti L, Cresta E, Cupini LM, Calabresi P, Sarchielli P, “The putative role of neuroinflammation in the complex pathophysiology of migraine: From bench to bedside,” Neurobiol. Dis., vol. 180, p. 106072, May 2023, doi: 10.1016/j.nbd.2023.106072.
- Iyengar S, Johnson KW, Ossipov MH, Aurora SK, “CGRP and the Trigeminal System in Migraine,” Headache, vol. 59, no. 5, pp. 659–681, May 2019, doi: 10.1111/head.13529.
- Peng KP, May A, “Migraine understood as a sensory threshold disease,” Pain, vol. 160, no. 7, pp. 1494–1501, Jul. 2019, doi: 10.1097/j.pain.000000000000153.1
- Benjamin T, Gillard D, Abouzari M, Djalilian HR, and Sharon JD, “Vestibular and auditory manifestations of migraine,” Curr. Opin. Neurol., vol. 35, no. 1, pp. 84–89, Feb. 2022, doi: 10.1097/WCO.0000000000001024.
- Vanneste S, Byczynski G, Verplancke T, Ost J, Song JJ, De Ridder D, “Switching tinnitus on or off: An initial investigation into the role of the pregenual and rostral to dorsal anterior cingulate cortices,” NeuroImage, vol. 297, p. 120713, Aug. 2024, doi: 10.1016/j.neuroimage.2024.120713.
- De Ridder D, Vanneste S, Langguth B, Llinas R, “Thalamocortical Dysrhythmia: A Theoretical Update in Tinnitus,” Front. Neurol., vol. 6, p. 124, 2015, doi: 10.3389/fneur.2015.00124.
- Fern J, ez-Sola, “Central Sensitization: A Pathogenic Mechanism in Complex Undefined Diseases,” vol. 9, no. 6, pp. 2485–2490, Dec. 2019, doi: 10.37532/1758-2008.2019.9(6).599.
- De Meulemeester K, Meeus M, De Pauw R, Cagnie B, Keppler H, Lenoir D, “Suffering from chronic tinnitus, chronic neck pain, or both: Does it impact the presence of signs and symptoms of central sensitization?,” PloS One, vol. 18, no. 8, p. e0290116, 2023, doi: 10.1371/journal.pone.0290116.
- Jastreboff PJ, Gray WC, Gold SL, “Neurophysiological approach to tinnitus patients,” Am. J. Otol., vol. 17, no. 2, pp. 236–240, Mar. 1996.
- De Ridder D, Vanneste S, Smith M, Adhia D, “Pain and the Triple Network Model,” Front. Neurol., vol. 13, p. 757241, 2022, doi: 10.3389/fneur.2022.75724.1
- Isler B, et al., “Lower glutamate and GABA levels in auditory cortex of tinnitus patients: a 2D-JPRESS MR spectroscopy study,” Sci. Rep., vol. 12, no. 1, p. 4068, Mar. 2022, doi: 10.1038/s41598-022-07835-8.
- Le Prell CG, Hughes LF, Dolan DF, Bledsoe SC, “Effects of Calcitonin-Gene-Related-Peptide on Auditory Nerve Activity,” Front. Cell Dev. Biol., vol. 9, p. 752963, Nov. 2021, doi: 10.3389/fcell.202.1752963.
- Norena AJ, “The Analogy between Tinnitus and Chronic Pain: A Phenomenological Approach,” Brain Sci., vol. 13, no. 8, p. 1129, Jul. 2023, doi: 10.3390/brainsci13081129.
- Ji RR, Nackley A, Huh Y, Terrando N, Maixner W, “Neuroinflammation and Central Sensitization in Chronic and Widespread Pain,” Anesthesiology, vol. 129, no. 2, pp. 343–366, Aug. 2018, doi: 10.1097/ALN.0000000000002130.
- Umemoto KK, Tawk K, Mazhari N, Abouzari M, Djalilian HR, “Management of Migraine-Associated Vestibulocochlear Disorders,” Audiol. Res., vol. 13, no. 4, pp. 528–545, Jul. 2023, doi: 10.3390/audiolres13040047.
- Abouzari M, Tawk K, Kim JK, Larson ED, Lin HW, Djalilian HR, “Efficacy of Nortriptyline-Topiramate and Verapamil-Paroxetine in Tinnitus Management: A Randomized Placebo-Controlled Trial,” Otolaryngol Head Neck Surg. Off. J. Am. Acad. Otolaryngol Head Neck Surg., Nov. 2024, doi: 10.1002/ohn.1063.
- Ghorbani Z, et al., “The effects of vitamin D supplementation on interictal serum levels of calcitonin gene-related peptide (CGRP) in episodic migraine patients: post hoc analysis of a randomized double-blind placebo-controlled trial,” J. Headache Pain, vol. 21, no. 1, p. 22, Feb. 2020, doi: 10.1186/s10194-020-01090-w.
- Goshtasbi K, Tawk K, Khosravi P, Abouzari M, Djalilian HR, “Smartphone-Based Cognitive Behavioral Therapy and Customized Sound Therapy for Tinnitus: A Randomized Controlled Trial,” Ann. Otol. Rhinol. Laryngol., vol. 134, no. 2, pp. 125–133, Feb. 2025, doi: 10.1177/00034894241297594.