Is a Public/Private Split the Ideal Way to Practice?
Working a dual public/private model in New Zealand offers opportunities to teach and handle complex cases together with the sense of control that comes with private practice.
Christopher E. Kennel, MD
About 18 years ago, my wife and I spent six weeks in Croatia, exploring her family heritage. We fell in love with the Mediterranean climate. So, during my residency training, I searched for places that would offer a similar climate where I could also work as an otolaryngologist. With a blend of luck, initiative, and blind faith, we moved our family of four to Hawke’s Bay, New Zealand, in 2022.
 Christopher E. Kennel, MD
Christopher E. Kennel, MD

This April, with the Medical Council’s blessing, I began working 50% privately and 50% publicly (this is the most common surgical practice model here). I've encountered aspects of private practice in New Zealand that some of my colleagues in the United States and elsewhere may find interesting.
First, I have really enjoyed the administrative side of private practice because I finally feel in control of my destiny. Setting fees, negotiating with insurers, working on office efficiency, and even trademarking a logo have helped me discover my inner entrepreneur. I was honestly surprised by the spring in my step that came from showing up to a clinic where I'm a director rather than an employee. Our public and private facilities are the same (we have a public-private hybrid arrangement because our public hospital does not have physical space for ENT). Yet, since starting private practice, I have felt more empowered to make changes to my clinic spaces to improve patients’ experiences than when I was doing public-only work.
Negotiation with insurers has been surprisingly reasonable. Most insurers approved my prices for clinic and surgery services, which I generated by creating a model that incorporates staff time, equipment, post-op care, other overhead, disposables, plus a desired hourly profit for clinic and theatre work. The major insurer in New Zealand prefers to negotiate for “affiliated provider” pricing. I asked for and received their average prices for otolaryngologists in the country as a frame of reference. Some of their clinic prices were a bit lower than I preferred, but the advantage to accepting the lower prices is that they pay within 24 hours of a patient visit. The contract is also flexible because I do not have to provide any service for which we could not agree upon a price.
Our EMR is easy to use and designed for doctors. It has been the single most important mental energy boost I have experienced. It is cloud-based, fast, reliable, and integrated with Xero for accounting. I can do more in less time than I could publicly or in the US. I cannot overstate how much happier I am using IT that just works.
Because there is no tort system in New Zealand, and we have the ACC that compensates everyone for injuries (e.g., auto accidents, sports accidents, medical complications), indemnity insurance is only about $500 USD per year. We do not need to practice defensive medicine, though we all need to have a structured audit process to track surgical outcomes and ensure quality of care.
We run a lean system. The expectation is that a clinic visit generates a letter to a GP, referrer, or patient when self-referred. There is no need to capture extra data. I share a secretary that checks in our patients. I have one clinic room with a computer, desk, and equipment. After checking in, a patient sees me (no medical assistant or nurse is needed to gather info), and then I write a simple letter. It may be a few sentences for something minor or paragraphs if there is a more complex issue. There are no rules about what it must state, and I can attach photos to show important findings. My structure has a diagnosis, advice, proposed treatment, and a brief commentary. After seeing me, the patient stops by our receptionist to pay and make a follow-up visit, if needed. Because we do not need to employ many people, we can afford to do private practice on a part-time basis.

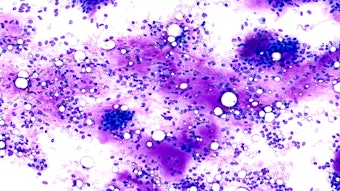
My schedule starts at 8:30 am and ends around 4:30 pm. On most days, I see 14 to 16 patients in clinic. Skin cancer is a big problem here because of the low air pollution and outdoor lifestyle. There are not enough surgical dermatologists so the public system contracts with us privately to manage most complex facial skin cancer. These visits tend to be quick, making for relaxed clinic days. As a result, I can afford to spend 40 minutes with a complex migraine patient when needed. The skin cancer contract has helped me ramp up immediately and stay busy while I build a private ENT surgical waiting list.

Call is done publicly. Oral maxillofacial surgery handles all trauma except for nasal fractures. Most of the time, we have residents taking first call, and we get paid a modest amount for call up to 1:6. Since there are only three of us in the call pool, the public system hires locums to support our 1:6 call schedule. But if we want to augment our income, we can also take these locums shifts for about 10 times the basic call rate. The call burden is reasonable, so it is a good arrangement.
Unlike in the US, I had to find my own anesthesiologist to work with privately. Prior to starting private practice, I started keeping tabs on which ones seemed comfortable and efficient with ENT procedures. Anesthesiologists manage all post-op pain and prescriptions for my patients—it gives them something to do while I am operating.
Public specialists are unionized here, and last year they went on strike for better pay and benefits. Residents are unionized, too. (They are currently in the midst of various strike actions.) And New Zealanders are quite supportive of striking for better pay and working conditions in the public sector.
Finally, since starting private practice, I have felt empowered to cut through the red tape and make things happen. In the public sector, I had to follow certain formularies and could only use things that the hospital could acquire for me. Privately, I have been able to import concentrated dexamethasone (24mg/mL) for intratympanic injections, get ear powders compounded, and so on. I plan to start offering SLIT this year. (There is no one offering immunotherapy in our region.) And I may start a side project importing ENT equipment that currently is not available in the country.
I feel lucky to have a hybrid opportunity where I can teach and handle complex cases on the public side, yet experience the sense of control and entrepreneurship that comes with private practice. I would encourage any trainee or early-career otolaryngologist to explore private practice opportunities. Who knows, you may have an inner entrepreneur waiting to be discovered. And if you would like a major change, check out New Zealand—if you are younger than 55 since that is the cutoff age to immigrate here.