A Novel, AI-Based Method of Mitigating Prior Authorization Denials
Using ethical AI to create a model that can help surgeons mitigate prior authorization denials, increase first-pass approvals, and decrease peer-to-peer events, to benefit surgeons, staff, and their patients.
Bradford G. Bichey, MD, MPH
(See author’s disclosures at the end of this article.)
2021 was the start of my understanding of the early implications of artificial intelligence (AI) in our sector. At that time, I was leading a health tech startup focused on enhancing communications between surgeons and patients. We had just begun to implement real-time analysis to deepen our understanding of the patient journeys facilitated through our platform. This was prior to the widespread release of technologies such as ChatGPT, large language models (LLMs), and AI.
The Ethical Dilemma of AI in Healthcare
I felt both fearful and hopeful then. Would we see a new era of efficiency and innovation or something else, more akin to the promise of electronic health records (EHRs) that never materialized? Today, it is evident that AI frameworks have become increasingly pervasive in the insurance industry. Unfortunately, as AI has been used by large insurance corporations over the last five years, its application has triggered significant ethical concerns. Recent allegations suggest that some corporations have been using AI to deny patient claims, ostensibly putting profit ahead of patient care. This has led to a series of lawsuits1,2 as insurance providers have not delivered on their promise of better healthcare.
A Lack of Transparency Across the Industry
There is no doubt that insurance companies have been using these AI systems to analyze claims for some time. A recent class-action lawsuit filed in Sacramento accuses Cigna of using an AI system, PxDx, to undercut costs by denying claims. In this instance, the lawsuit alleges that Cigna denied close to 300,000 claims with an average review time of 1.2 seconds. ‘“We literally click and submit,” one former Cigna doctor said. “It takes all of 10 seconds to do 50 at a time.”1 UnitedHealthcare is also facing accusations of using flawed AI to deny Medicare claims, capitalizing on the low likelihood of appeals from senior patients. A recent lawsuit claims that UnitedHealth’s use of the “nH Predict” algorithm violates contracts with patients and the insurance laws of numerous states.2 Because the systems in question were both powerful and hidden, by 2022, I began deconstructing the algorithms designed to evaluate and block surgical prior authorization (PA) documentation using a team of experts.
Defenses of AI Use by the Insurance Industry
Despite the controversy, some defend the technology being used to deny claims. They cite studies where AI systems have matched or even exceeded human doctors in diagnostic accuracy. Some published studies have shown AI’s potential in improving diagnostic precision and patient interaction quality.3 As another example, Google’s Med-PaLM 2 (an LLM) has recently showcased remarkable capabilities, achieving over 85% accuracy on simulations styled after the United States Medical Licensing Examination.4 AI-driven PA determinations claim to comprehensively assess patient health indicators with high accuracy. However, as surgeons, we are well aware that accurate diagnosis is foundational to positive patient outcomes, and that direct human interaction is implicitly necessary.
Unethical AI Use Takes Advantage of Provider Burnout
Accuracy aside, the crux of the issue remains that insurers are misusing AI by leveraging the technology to obstruct rather than enhance patient care. This misuse underscores a broader systemic problem within healthcare, where efficiency tools are repurposed for profit at the expense of patient access to necessary treatments. AI discussions are not always popular in my meetings with surgeons. It is a problem exacerbated by overwork and a reluctance to embrace the rapid changes we are currently seeing in healthcare. Skepticism plays a key role in the slow adoption we are experiencing. A recent Medscape Physician and AI Report surveyed over 1,000 U.S. physicians about their views on AI. Across those surveyed, 65% had concerns about AI making diagnosis and treatment decisions, while 56% of respondents expressed enthusiasm about having AI as an assistant in their practice.5
Recently, Alfredo A. Sadun, MD, PhD, the Flora L. Thornton Endowed Chair at Doheny Eye Centers, UCLA and Vice Chair of the UCLA Ophthalmology Department, commented on how burnout and other factors are also driving the slow adoption of AI solutions by physicians. 6 “There’s still an abysmally poor understanding of AI among physicians in general. It's striking because these are intelligent, well-educated people. But we tend to draw conclusions based on what we're familiar with, and most doctors’ experience with computers involves EHRs and administrative garbage. It’s the reason they’re burning out,” said Dr. Sadun.6
Legal Versus Ethical Practices in Surgery
The hours of work we do to document care justifying a case can now depend on a 1.2-second software review. Figure 1 shows the massive increase in UnitedHealthcare Group’s (UHG) revenue per UnitedHealth (UH) insured patients over a 5-year period ending in 2023. “nH Predict” algorithms were in use at or before 2020.
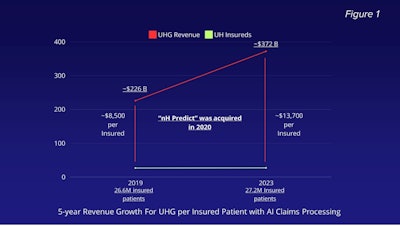 Figure 1. UnitedHealthcare Group’s (UHG) revenue per UnitedHealth (UH) insured patients over a 5-year period ending in 2023.
Figure 1. UnitedHealthcare Group’s (UHG) revenue per UnitedHealth (UH) insured patients over a 5-year period ending in 2023.
Unfortunately, it’s clear that claim denial en masse has become a tactical move to place profitability over patient care in some instances.7-11 This behavior is in direct contrast to the stated public mission of some of these companies. UnitedHealth Group’s core mission statement can be found on its website: “Our mission is to help people live healthier lives. Our role is to help make healthcare work better for everyone. We seek to enhance the performance of the health system and improve the overall health and well-being of the people we serve and their communities.”12
Whether or not such practices are legal, healthcare insurers dictating care is undoubtedly unethical. Currently, insurance companies are exploiting circumstances in which overburdened surgical teams are unable to produce documentation that meets obscure AI scoring criteria. It is a practice that blocks at least 13% of the care that should be covered. These findings were brought to light when the U.S. Department of Health and Human Services (HHS) inspected claim denials for Medicare Advantage plans in 2022.13,14
Designing AI Mitigation for PA Denials
In 2022, in response to what we were learning, the question arose, “Can we use ethical AI to create a solution that effectively helps all surgeons mitigate PA denials, increase first pass approvals, and decrease peer-to-peer events, to the benefit of surgeons, staff, and patients?”
Core Vision
In the current healthcare market, where human oversight is increasingly assisted by AI, it is time for surgeons to begin embracing AI not just as a tool but as a core component of their operational strategies. For the PA process, this AI-driven approach offers a dual benefit of enhanced likelihood of approval and increased patient access to care, leading to more ethical outcomes.
Major Concepts
Transforming the challenges posed by insurance companies into opportunities to enhance surgical care necessitates a strategy that incorporates four key concepts.
- Increasing the Likelihood of Surgical Care
By adopting AI-driven systems to improve documentation submitted to insurance companies, it is important to use algorithms to analyze patient data against a set of criteria that closely mirrors insurance prerequisites for approvals. By ensuring all necessary conditions and documentation are met before submission, these systems significantly increase the likelihood of approval for surgeries. - Decreasing Administrative Burden on Clinical Staff
Administrative tasks related to PAs are complex, notoriously time-consuming, and prone to errors and frustration. By implementing AI to handle these tasks clinical staff have more time to focus more on patient care rather than these administrative duties. - Decreasing the Risk of Audit Repayments (Addressing the Template Problem)
Audit repayments often occur when insurers detect discrepancies in billing and documentation for provided services. Templated documentation does not accurately reflect the individualized patient care delivered. To combat this, AI ensures that records are both accurate and comprehensive. By eliminating templates, AI reduces the risk of post-audit discrepancies and potential repayments. - Ensuring 100% HIPAA Compliance
Compliance with HIPAA’s privacy and security regulations is critical in all healthcare processes, especially those involving the extensive use of patient data with AI. Built-in compliance and monitoring become programmatic, anonymizing patient identifiers where necessary, ensuring that all patient information is handled in compliance with federal regulations.
Using these four concepts, it is possible to effectively reverse-engineered the PA process into a beneficial tool that supports surgical care delivery and increases patient access to surgical services.
The Sinus Procedure Blueprint
Figure 2 outlines the basic agents, systems, and processes used in creating surgical PA documentation. To create documentation that mitigates denials through an upscoring process, several different types of AI are used in a process designed around humans-in-the-loop (that is, the selective inclusion of humans in the process rather than their complete exclusion).
 Figure 2. The basic agents, systems, and processes used in creating surgical PA documentation.
Figure 2. The basic agents, systems, and processes used in creating surgical PA documentation.
Figure 3 below illustrates the process of upscored note creation using four major steps. These steps can be used for any blueprinted surgical procedure. The steps are as follows:
- Integrated Upload
This step ensures the effortless integration of patient data into the AI system, allowing for quick uploads directly from healthcare providers’ EHRs. - ICD-10 Baselining
The AI framework employs analysis of International Classification of Diseases, Tenth Revision (ICD-10) codes.15 Predictive analytics are used to baseline diagnoses ensuring compliance with insurance requirements critical for reducing mismatches and discrepancies that could lead to claim denials. - Deficiency Detection/Upscoring
The AI analyzes the uploaded documents, cross-referencing patient data against a comprehensive checklist based on insurer requirements. Upon detecting deficiencies, the AI suggests corrections and enhancements. Upscoring involves refining the documentation to better demonstrate medical necessity for the procedures requested. - Note Creation/Quality Improvement
After adjustments, the generative AI creates an upscored medical note for download. This document is optimized for approval and addresses all previously identified gaps, better aligning with payer expectations. To ensure continuous improvement, the AI also conducts post-process analyses used to refine future algorithms.
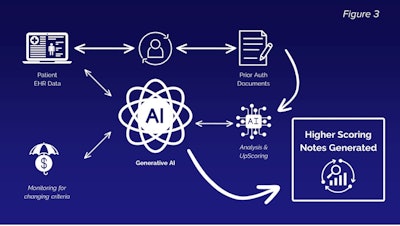 Figure 3. The process of upscored note creation.
Figure 3. The process of upscored note creation.
By leveraging AI in these ways, this framework not only reduces the administrative burden on healthcare providers but also enhances the accuracy and efficiency of the PA process.
Outcomes and Conclusions
To date, our framework has analyzed approximately 12,000 patient journeys. Approximately 20% have undergone note creation through the sinus procedure blueprint based on patient candidacy. Our peer-to-peer reviews have been remarkably low, occurring in fewer than one out of every 200 cases, and the rate of first-pass denials stands at an impressive 2% across the dataset.
Figure 4 illustrates the improvement achievable in ICD-10 scoring. Scoring is indicative of the probability that the patient has the specified diagnosis predicting hundreds of j-codes per patient.
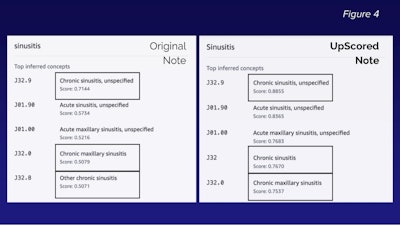 Figure 4. The potential improvement achievable in ICD-10 scoring.
Figure 4. The potential improvement achievable in ICD-10 scoring.
These outcomes indicate a substantial enhancement over existing models, even within this relatively limited dataset. We anticipate that further refinements and the development of additional surgical procedure blueprints will continue to drive improvements in these outcomes.
As healthcare professionals and industry leaders, we all must scrutinize the role of AI in healthcare. It is imperative to ensure that these tools are used to support, rather than undermine, patient care. AI holds tremendous potential to transform healthcare, but its application must be guided by ethical standards that prioritize patient well-being. Now more than ever, surgeons and their stakeholders need to be involved in rethinking their strategic processes.
I personally invite all healthcare professionals to join me by adopting AI solutions that are transparent, equitable, and patient-centered, ensuring technology serves as a bridge to better health outcomes, not a barrier.
Disclosure: Dr. Bichey is the founder of Indiana Sinus Centers, and founder/CEO of Nemedic, Inc.
Disclaimer: The model described in this article is currently under development and may be offered in the future as a paid product or a service accompanying a paid product. This article does not constitute the endorsement of any product, and all opinions are those of the author and may or may not be shared by the AAO-HNS.
References
- Rucker, P., Miller, M. and Armstrong, D. “How Cigna Saves Millions by Having Its Doctors Reject Claims Without Reading Them.” ProPublica, 2023. : https://www.propublica.org/article/cigna-pxdx-medical-health-insurance-rejection-claims
- Payerchin, Richard. “UnitedHealthcare Used AI to Deny Patients’ Health Insurance Coverage, Lawsuit Says.” Medical Economics, November 16, 2023. https://www.medicaleconomics.com/view/unitedhealthcare-used-ai-to-deny-patients-health-insurance-coverage-lawsuit-says.
- Huang, Andy S., Kyle Hirabayashi, Laura Barna, Deep Parikh, and Louis R. Pasquale. “Assessment of a Large Language Model’s Responses to Questions and Cases About Glaucoma and Retina Management.” JAMA Ophthalmology 142, no. 4 (April 1, 2024): 371–75. https://doi.org/10.1001/jamaophthalmol.2023.6917.
- Google Research. “Med-PaLM,” n.d. https://sites.research.google/med-palm/.
- McKenna, John. “Medscape Physicians and AI Report 2023: A Source of Help or Concern?” Medscape, October 30, 2023. https://www.medscape.com/slideshow/2023-artificial-intelligence-6016743.
- Kita, Joe. “Are You Ready for AI to Be a Better Doctor Than You?” Medscape, April 12, 2024. https://www.medscape.com/viewarticle/are-you-ready-ai-be-better-doctor-than-you-2024a100070q?form=fpf.
- UnitedHealth Group. “UnitedHealth Group Reports 2018 Results Highlighted By Continued Strong And Diversified Growth,” January 15, 2019.
- UnitedHealth Group. “UnitedHealth Group Reports Fourth Quarter and Full Year 2023 Financial Results,” January 12, 2024. https://www.unitedhealthgroup.com/newsroom/2024/2024-01-12-uhg-reports-fourth-quarter-results.html.
- Jaffe, Susan. “Feds Rein in Predictive Software That Limits Care for Medicare Advantage Patients,” Health News Florida, October 6, 2023.
- UnitedHealth Group. “UnitedHealth Group Reports 2019 Results,” January 15, 2020.
- UnitedHealth Group. “UnitedHealth Group Investor Conference 2023,” n.d. https://www.unitedhealthgroup.com/investors/conference.html#unitedhealthcare.
- UnitedHealth Group. “Helping People Live Healthier Lives and Helping Make the Health System Work Better for Everyone.” UnitedHealth Group, 2024. https://www.unitedhealthgroup.com/people-and-businesses/mission-values.html.
- Christi Grimm. “Some Medicare Advantage Organization Denials of Prior Authorization Requests Raise Concerns About Beneficiary Access to Medically Necessary Care.” U.S. Department of Health and Human Services Office of Inspector General, April 2022. https://oig.hhs.gov/oei/reports/OEI-09-18-00260.pdf.
- U.S Department of Health and Human Services Office of Inspector General. “(Summary) Some Medicare Advantage Organization Denials of Prior Authorization Requests Raise Concerns About Beneficiary Access to Medically Necessary Care,” April 27, 2022.
- World Health Organization. “International Classification of Diseases Tenth Revision (ICD-10)”. World Health Organization, 2019. Available at: https://icd.who.int/browse10/2019/en