Enhancing Patient Care through Data-Driven Practice
Exploring the intersection of quality improvement, evidence-based medicine, and the Reg-ent clinical data registry.
Anirudh Saraswathula, MD, MS, Patient Safety Quality & Improvement (PSQI) Committee member, Prasanth Pattisapu, MD, MPH, Outcomes Research and Evidence-Based Medicine (OREBM) Committee member, Vikas Mehta, MD, MPH, Coordinator for Research and Quality, Soham Roy, MD, MMM, Chair, PSQI Committee, and Michael J. Brenner, MD, Chair, OREBM Committee
Otolaryngology, much like other medical specialties, constantly seeks innovative ways to enhance patient care and improve outcomes. Three key entities within the American Academy of Otolaryngology–Head and Neck Surgery and its Foundation (AAO-HNS/F) are central to these efforts: the Patient Safety & Quality Improvement (PSQI) Committee, the Outcomes Research and Evidence-Based Medicine (OREBM) Committee, and the Reg-ent Clinical Data Registry. This article explores the interrelationship of these entities and their collective impact on patient care, as well as implications for health equity, adoption of technologies, and evolving clinical practice standards.
Understanding the Players
The PSQI Committee is charged with raising awareness within the Academy regarding patient safety and quality improvement issues. It engages committee members in projects and presentations that improve the quality of care in otolaryngology-head and neck surgery. The committee educates Academy members about evidence-based guidelines, practice standards, and other systems that enhance care. It also identifies products, tools, services, and processes that lead to safer care of otolaryngology-head and neck surgery patients, assisting the Academy in making them known and available to its membership. It also has an extensive portfolio of safety and quality-related initiatives.
The OREBM Committee contributes expertise on health services research and evidence-based medicine. The committee is also responsible for developing and maintaining educational materials, panels, courses, and other resources that helps members stay informed about the latest research and evidence-based practices. The committee curates the evidence, ensuring that clinical practice is grounded in the best available evidence, leading to improved patient outcomes. OREBM partners with the PSQI Committee in providing input to clinical practice guidelines and ideas for clinical data registry priority areas, along with a range of presentations and projects.
Reg-ent, an otolaryngology-specific clinical data repository, has over 50 million patient visits from 10 million patients. It allows for quality data reporting to the Centers for Medicare & Medicaid Services’ Merit-Based Incentive Payment System (MIPS) and MIPS Value Pathways (MVPs) and now offers the capability for research and quality improvement projects. The Reg-ent Research Advisory Group (RRAG) evaluates proposed studies submitted by participating practices and AAO-HNSF committees to utilize de-identified data sets from the registry to answer research questions, drive quality improvement projects, and enhance patient care across the specialty. Reg-ent supports tracking patient care, connecting outcomes with processes, and meeting third-party payer requirements. In addition to MIPS/MVPs, Reg-ent is also developing a process that allows participants at large hospital systems to track performance and benchmark against peers for certain quality metrics (i.e. postoperative hemorrhage, 30-day readmission, length of stay, etc.) available through a dashboard, facilitating continuous improvement in clinical practice. The data is also being utilized on a national level to bolster advocacy efforts by the AAO-HNS in discussions with CMS and private insurance entities and promote the interests of our patients and our specialty as a whole.
How Does Evidence-Based Medicine Relate to Safety and Quality?
Evidence-Based Medicine (EBM) is complementary to that of Patient Safety and Quality Improvement (PSQI). Whereas EBM focuses on "doing the right things" based on research evidence, QI emphasizes "doing things right" through local processes (see the figure below). Taken together, these approaches can be integrated to the ideal of "doing the right things the right way." Understanding the differences and similarities between EBM and QI makes it possible to combine best evidence with practical improvements in clinical settings, as is emphasized in AAO-HNSF Clinical Practice Guidelines that use rigorous standards to synthesize evidence and apply it to quality improvement opportunities.
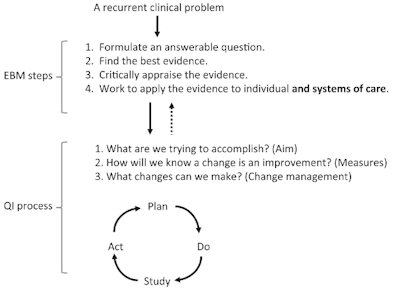 This figure has been adapted from Figure 1 Relationships Between Quality Improvement (QI) and Evidence-Based Medicine (EBM) in Glasziou P, Ogrinc G, Goodman S (2011).
This figure has been adapted from Figure 1 Relationships Between Quality Improvement (QI) and Evidence-Based Medicine (EBM) in Glasziou P, Ogrinc G, Goodman S (2011).
Both committees have contributed guideline proposals and participated in guideline development. EBM emphasizes the synthesis of research to guide clinical decisions but does not always emphasize practical implementation. Conversely, QI focuses on addressing systemic issues in healthcare delivery but may lack the rigorous evidence base that EBM provides. The integration of EBM and QI requires a balanced approach that emphasizes evidence-based actions and systematic improvements to ensure effective and reliable healthcare delivery. Data-driven improvements are central to the intersection of the PSQI Committee, OREBM Committee, and Reg-ent. All three groups promote best practices for data collection and analysis (such as transparent data display and maximizing accessibility to staff, patients, and families) to foster accountability and continuous improvement.
Health Equity and Diversity, Equity, and Inclusion (DEI)
Health equity and DEI are integral to quality improvement efforts, and an equity lens is increasingly applied to evidence-based analyses. The Healthy People 2030 Initiative set forth by the U.S. Department of Health and Human Services defines goals to eliminate health disparities, achieve health equity, and enhance health literacy. Health equity can be integrated into research by engaging a diverse group of stakeholders throughout the research process, examining upstream factors related to differences in social groups, promoting representative enrollment in clinical trials, assessing treatment effects across populations, investigating difference in retention, and using tools such as PROGRESS-PLUS or equity extensions in research. Addressing the social determinants of health (SDoH) are also a critical aspect of otolaryngology care. The Centers for Medicare & Medicaid Services (CMS) now require participants in the Hospital Inpatient Quality Reporting Program to screen for food insecurity, housing instability, transportation needs, difficulties with utilities, and safety that can serve as triggers for referrals.
The OREBM and PSQI Committees emphasize the importance of addressing disparities in healthcare outcomes. Stratifying quality data based on demographics and involving diverse perspectives can improve quality improvement projects. For example, analyzing patient outcomes across different demographic groups can reveal disparities that may require targeted interventions. Also, using more “real-world” data through registries such as Reg-ent allows our specialty to further explore external validity of research study results, thereby improving our understanding of otolaryngology care in all populations. Through these efforts, OREBM, PSQI, and Reg-ent can support the development of multilevel interventions needed for addressing the roots of health disparities and promoting health equity.
Adapting to New Technology and Innovation
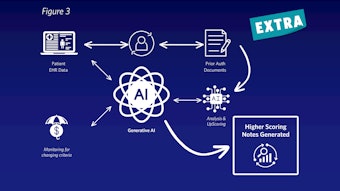
The PSQI and OREBM Committees are also staying abreast of new technologies, including artificial intelligence (AI), that offer significant potential for enhancing patient care. AI can be used for predictive analytics and decision support, helping healthcare providers identify high-risk patients and tailor interventions accordingly. Innovations in data collection and patient monitoring also enable more precise and timelier care. AI-driven predictive models can improve the accuracy of diagnoses and treatment plans, potentially leading to better patient outcomes. Similarly, advanced monitoring technologies can provide real-time data, allowing for more responsive and effective care. The potential enhancements in precision medicine, clinical decision support, and practice optimization are substantial; however, concerns of health equity, privacy, and bias require thoughtful management.
Several challenges remain in integrating quality improvement, evidence-based medicine, and registry data into practice. Common barriers include limited access to real-time data, resistance to change among healthcare providers, and the complexity of implementing new technologies. Additionally, large clinical databases like Reg-ent, quality improvement processes, and adoption of evidence-based best practices often require significant time, engagement, and resources to be broadly accepted within the clinical community.
To address these challenges, the committees emphasize the importance of ongoing education, collaboration, and the use of adaptive strategies. Future directions include exploring new technologies and methodologies to disseminate improvements in care. The use of implementation science frameworks and alternative approaches to disseminating knowledge such as social media platforms, use of immersive technology, and novel approaches to engaging colleagues may open new opportunities. The AAO-HNS has been working diligently to continue to support these efforts through the two committees, the Reg-ent database, and other activities such as the continued development of clinical practice guidelines.
Reg-ent Data, Clinical Practice Guidelines, Performance Measures
Translating evidence into action and improving care are cornerstones of the high-quality care. These efforts reinforce the mission of the AAO-HNSF: “To engage our members and help them achieve excellence and provide high-quality, evidence-informed, and equitable ear, nose, and throat care through professional and public education, research, and health policy advocacy, as well as its vision to be the global leader in optimizing quality ear, nose, and throat patient care.”
The PSQI and OREBM Committees provide proposals for clinical practice guidelines, and their members are represented in guideline development and peer review. Performance measures, in turn, play a key role in driving practice changes by providing benchmarks for quality care. Reg-ent offers a potentially powerful resource for generating evidence on the quality of care provided and outcomes.
The integration of best evidence with implementation science plays a critical role in advancing otolaryngology-head and neck surgery practice. Reg-ent and the Research and Quality infrastructure of the Academy provide vehicles for leveraging data-driven improvements, promoting health equity, assessing new technologies, and translating guidelines into practice. Collectively, member engagement with quality initiatives across private practice, academic practice, and military can enhance the quality and safety of patient care. Ongoing collaboration and innovation are essential to sustain these efforts and achieve the best possible outcomes for patients, and having our own specialty-specific data will be crucial in the future for us to achieve these aims.
Resources
Glasziou P, Ogrinc G, Goodman S. Can evidence-based medicine and clinical quality improvement learn from each other? BMJ Quality & Safety. 2011;20:i13-i17. doi: https://doi.org/10.1136/bmjqs.2010.046524
The U.S. Playbook to Address Social Determinants of Health. Whitehouse.Gov, Nov. 2023 www.whitehouse.gov/wp-content/uploads/2023/11/SDOH-Playbook-3.pdf, Date accessed: May 23, 2024
Megwalu UC, Raol NP, Bergmark R, Osazuwa-Peters N, Brenner MJ. Evidence-Based Medicine in Otolaryngology, Part XIII: Health Disparities Research and Advancing Health Equity. Otolaryngol Head Neck Surg. 2022 Jun;166(6):1249-1261. doi: 10.1177/01945998221087138. Epub 2022 Mar 22. PMID: 35316118.
Reg-ent℠ Clinical Data Registry - American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) (entnet.org)
Schmalbach CE, Brereton J, Bowman C, Denneny JC 3rd. American Academy of Otolaryngology-Head and Neck Surgery/Foundation Reg-ent Registry: Purpose, Properties, and Priorities. Otolaryngol Head Neck Surg. 2021 May;164(5):964-971. doi: 10.1177/0194599820984135. Epub 2021 Jan 12. PMID: 33433257.
Gómez, Cynthia A. PhD; Kleinman, Dushanka V. DDS, MScD; Pronk, Nico PhD, MA, FASCM, FAWHP; Wrenn Gordon, Glenda L. MD, MSHP, FAPA; Ochiai, Emmeline MPH; Blakey, Carter BS; Johnson, Ayanna MSPH; Brewer, Karen H. MPH. Addressing Health Equity and Social Determinants of Health Through Healthy People 2030. Journal of Public Health Management and Practice 27(Supplement 6):p S249-S257, November/December 2021. | DOI: 10.1097/PHH.0000000000001297
The AAO-HNS/F Committees Handbook, available at https://www.entnet.org/wp-content/uploads/2024/05/CommitteeHandbook_V8.pdf