An era of uncertainty in healthcare
No doubt about it. We are living in an era of uncertainty in healthcare. In medicine in the United States, we have been accustomed for decades to a system that has rewarded volume and intensity of services delivered.
By John H. Krouse, MD, PhD, MBA, Professor and Chairman, Otolaryngology-Head and Neck Surgery, Temple University School of Medicine and Editor in Chief, Otolaryngology–Head and Neck Surgery
No doubt about it. We are living in an era of uncertainty in healthcare. In medicine in the United States, we have been accustomed for decades to a system that has rewarded volume and intensity of services delivered. While the system has stimulated advances that have enhanced care of patients with acute medical illnesses, access to that care remains spotty and overall health, especially among the most vulnerable, generally lags behind most of the developed world. The cost of healthcare in the United States continues to skyrocket, with expenditures approaching $3 trillion in 2013, or almost 18 percent of the U.S. gross domestic product (GDP), significantly outpacing our nearest comparators. Obviously, this system is unsustainable in its present design.
In this era of uncertainty, transitions in healthcare are underway:
| TRANSITION FROM | TO |
| Fee-for-service | Bundled payments by networks and illnesses |
| Incentivized for volume |
Incentivized for value |
| Fragmented, individualized care |
Aligned, continuity of care |
| Acute hospital focus | Chronic outpatient disease management |
| Nonstandardized paper records | IT-based standardized records |
Given these transitions, we as otolaryngologists currently live in the “straddle” of this era of uncertainty. We continue to benefit from fee-for-service medicine, yet payer contracts are moving toward a greater emphasis on value, cost-reduction, and improved quality in processes and outcomes. Bundled payment arrangements and ACOs are on the horizon. Physicians continue to practice in an individualistic manner, although the influence of guidelines-based medicine is increasingly felt as a mechanism to decrease variation in care.
Unfortunately, it is in this straddle that we see adverse impact on physician revenue. Payments have declined as payers transition away from fee-for-service, yet incentives for quality are not in place to sufficiently offset this decline. Investment in IT infrastructure has been required, yet physicians have seen little return for this cost. It is unclear exactly how future payment systems will unfold, the timing of implementation, and how to advantageously position ourselves as otolaryngologist-head and neck surgeons.
In the future world of healthcare, the interface of health economics and physician practice is at the point of VALUE. In economic systems, the value of goods or services is understood as an interaction of the quality of those goods or services and the cost at which they are provided. In other words: VALUE = QUALITY ÷ COST.
Specific to healthcare, value can be created by increasing the quality of the care, decreasing the cost of the care, or some combination of both. Implicit in the discussion, however, is that consumers must be able to evaluate the quality of services provided, making public reporting of outcome data a necessary component of any value-based healthcare system. Physicians and health systems will need to create value propositions that reflect the needs of patients and their communities.
So what trends do we foresee? Healthcare will move toward increasing integration and expanded use of multidisciplinary teams. There will be greater transparency in price and quality, as well as mutual accountability with physicians and health systems. Rewards will be based on system outcomes rather than high volumes. At the physician level, incentives will be negotiated with health systems, and may be based on some combination of productivity and achievement of quality and service goals.
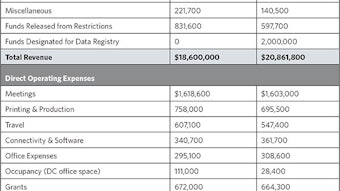
Otolaryngologist-head and neck surgeons need to be proactive in this era of uncertainty in healthcare. The AAO-HNSF is participating in the process of identifying low-value services through its “Choosing Wisely” campaign. It is interesting that just one of these 10 principles is specifically related to otolaryngology procedures. Future initiatives must be outcomes-based and define appropriate use of procedural interventions. Otolaryngologists must develop patient-centered quality indicators that define how and when care should be provided. Data and analytics will be critical, and the AAO-HNS is developing performance indicators and a comprehensive data registry that will assist in addressing these important issues of quality and value. Furthermore, Otolaryngology–Head and Neck Surgery will continue to expand its content in health policy and economics to support otolaryngologists as key partners in the care of their patients.
So, out of the chaos of this era of uncertainty comes the opportunity for leadership and proactive change. We must define evidence-based performance and quality metrics that allow us to thrive in the changing environment of health reform. We must engage patients and families in their care decisions, with the goals of increased satisfaction, improved outcomes, and reduced costs. With a sharp focus on quality, we, as otolaryngologists, can navigate healthcare uncertainty and take the lead in defining value in otolaryngology care.