Help Us Give Smiles (HUGS) Stage 1 and Stage 2 Microtia Repairs Using Autologous Rib, Primarily Nagata Technique
Jonathan C. Kopelovich, MD R5 Resident Physician University of Iowa Department of Otolaryngology Head and Neck Surgery Quito, Ecuador Ecuador Microtia Mission The 19-year-old father cocked his head to the side as the entire HUGS team gathered to see the excellent results of his prior stage 1 microtia repair. Unlike many of the children who came in for their first evaluation, hair hanging over their ears and avoiding eye contact, he stood proudly, had his hair cut short on the sides, tapered and lined as if to display to the world the ear he had so recently gained. He was proud to show it to us. We were proud to see it. This year he was set to undergo elevation of his framework to create a postauricular sulcus, lined with temporoparietal fascia and skin. He stood testament to the influence our intervention has on the lives of these young Ecuadorians. Ecuador has a population of 16 million, but for reasons not fully understood has six times the incidence of microtia, or congenital deformity of the ear, of nearby countries. Despite the incidence, these children are, per their parents’reports, castigated and made to feel awful by their peers. Microtia repair is a risky endeavor in the best of circumstances. The procedure is fraught with small, but important nuances that can make or break a result. Here, despite poor resources, we made big changes in the lives of our patients. Our team was deep and talented. We had six senior plastic surgeons, including Mack Cheney, MD, and Tessa Hadlock, MD, from the Massachusetts Eye and Ear Infirmary (MEEI) and Vito Quatela, MD, from Rochester, NY, the founders of this mission. A dermatologist and her fellow ran their own laser hair removal clinic for returning patients. The rest of the team included two anesthesiologists, four CRNAs, nine RNs, two medical students, three facial plastics fellows, and myself. We also had two administrators, one of whom additionally conducts research on the psychosocial outcomes of microtia repair. With a modicum of planning and lots of initiative, team members fell into the roles that best suited them. I rotated from table to table to help with rib harvests and wound closures, and helped manage the floor with a team consisting of a dedicated RN and a plucky medical student. The Ecuadorian hospital that hosted our mission had four operating rooms, two of which we occupied with our three surgical teams. An additional supply closet became the minor room—where the MEEI team churned through the myriad follow-up procedures that microtia patients require as they age. Here Dr. Hadlock narrated in English and Spanish for volunteers and patients while she operated under local using the light of her headlamp and a single mayo stand. The early part of the week was dedicated to our stage 1 repairs, while the latter half was devoted to second stage surgeries and other revisions. Our first and last days were devoted to intake and checkout respectively where we reviewed prior results and made plans for further procedures. In all, we performed more than 120 procedures. HUGS, as an organization, is well established and well run. Now in its 14th year, this organization has been returning to serve the population of Ecuador yearly and has more recently added humanitarian trips to Guatemala, Vietnam, and soon, Peru. These elite plastic surgeons continually push each other to improve and excel in the challenging realm of auricular reconstruction. The senior members have been coming for at least a decade and have warm relationships with each other, with the Ecuadorian physicians who host us, and with many of the children they have watched grow up. I was surprised by the sophisticated level of data collection and documentation. Each child was evaluated, measured, and photographed, and their surgical experience carefully indexed. The surgical approach is constantly evolving. Tracking outcomes has helped this team immensely to refine their approach and achieve uniform results. This team does not rest on its laurels; it is growing, expanding, and improving. I am proud to have been a part of such a world-class surgical team and am grateful to the AAO-HNSF Humanitarian Efforts Committee and HUGS Foundation for co-sponsoring my trip.
 Quito, Ecuador, and the Pichincha mountain.
Quito, Ecuador, and the Pichincha mountain.Jonathan C. Kopelovich, MD
R5 Resident Physician
University of Iowa Department of Otolaryngology Head and Neck Surgery
Quito, Ecuador
Ecuador Microtia Mission
The 19-year-old father cocked his head to the side as the entire HUGS team gathered to see the excellent results of his prior stage 1 microtia repair. Unlike many of the children who came in for their first evaluation, hair hanging over their ears and avoiding eye contact, he stood proudly, had his hair cut short on the sides, tapered and lined as if to display to the world the ear he had so recently gained. He was proud to show it to us. We were proud to see it. This year he was set to undergo elevation of his framework to create a postauricular sulcus, lined with temporoparietal fascia and skin. He stood testament to the influence our intervention has on the lives of these young Ecuadorians.
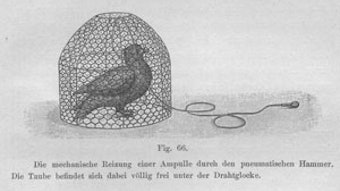
 Cartilaginous framework for stage 1 Nagata microtia repair.
Cartilaginous framework for stage 1 Nagata microtia repair.Ecuador has a population of 16 million, but for reasons not fully understood has six times the incidence of microtia, or congenital deformity of the ear, of nearby countries. Despite the incidence, these children are, per their parents’reports, castigated and made to feel awful by their peers. Microtia repair is a risky endeavor in the best of circumstances. The procedure is fraught with small, but important nuances that can make or break a result. Here, despite poor resources, we made big changes in the lives of our patients.
Our team was deep and talented. We had six senior plastic surgeons, including Mack Cheney, MD, and Tessa Hadlock, MD, from the Massachusetts Eye and Ear Infirmary (MEEI) and Vito Quatela, MD, from Rochester, NY, the founders of this mission. A dermatologist and her fellow ran their own laser hair removal clinic for returning patients. The rest of the team included two anesthesiologists, four CRNAs, nine RNs, two medical students, three facial plastics fellows, and myself. We also had two administrators, one of whom additionally conducts research on the psychosocial outcomes of microtia repair. With a modicum of planning and lots of initiative, team members fell into the roles that best suited them. I rotated from table to table to help with rib harvests and wound closures, and helped manage the floor with a team consisting of a dedicated RN and a plucky medical student.
 Brothers with microtia, their parents, and Dr. Kopelovich.
Brothers with microtia, their parents, and Dr. Kopelovich.The Ecuadorian hospital that hosted our mission had four operating rooms, two of which we occupied with our three surgical teams. An additional supply closet became the minor room—where the MEEI team churned through the myriad follow-up procedures that microtia patients require as they age. Here Dr. Hadlock narrated in English and Spanish for volunteers and patients while she operated under local using the light of her headlamp and a single mayo stand. The early part of the week was dedicated to our stage 1 repairs, while the latter half was devoted to second stage surgeries and other revisions. Our first and last days were devoted to intake and checkout respectively where we reviewed prior results and made plans for further procedures. In all, we performed more than 120 procedures.
HUGS, as an organization, is well established and well run. Now in its 14th year, this organization has been returning to serve the population of Ecuador yearly and has more recently added humanitarian trips to Guatemala, Vietnam, and soon, Peru. These elite plastic surgeons continually push each other to improve and excel in the challenging realm of auricular reconstruction. The senior members have been coming for at least a decade and have warm relationships with each other, with the Ecuadorian physicians who host us, and with many of the children they have watched grow up. I was surprised by the sophisticated level of data collection and documentation. Each child was evaluated, measured, and photographed, and their surgical experience carefully indexed. The surgical approach is constantly evolving. Tracking outcomes has helped this team immensely to refine their approach and achieve uniform results. This team does not rest on its laurels; it is growing, expanding, and improving. I am proud to have been a part of such a world-class surgical team and am grateful to the AAO-HNSF Humanitarian Efforts Committee and HUGS Foundation for co-sponsoring my trip.