Thyroid Surgery in Migori, Kenya
Dunia Abdul-Aziz, MD Harvard Otolaryngology Program Boston, MA The singing of children greeted us. After an eight-hour journey through the magnificent Rift Valley, we drove up to the gates of a walled compound in Migori, Kenya—a welcome sign to Brittany’s Home of Grace inviting us in. In February, a team from the Massachusetts Eye and Ear Infirmary, Boston, composed of American Academy of Otolaryngology—Head and Neck Surgery members Gregory W. Randolph, MD; Paul Konowitz, MD; David J. Lesnik, MD; and myself, and surgical nurse Nancy Kotzuba, RN, joined nurses, anesthesiologists and local staff of KenyaRelief.org in a weeklong effort, with a goal of providing medical and surgical care to patients with head and neck disease, particularly goiters. The experience highlighted the power, the potential, and the challenges of international humanitarian initiatives. This was our first time in Kenya, a country of about 39.4 million people, where the average income is slightly more than $2 a day1. We planned a thyroid mission to tackle endemic goiters, which remain prevalent despite salt iodization and Kenya’s status as the largest regional supplier of iodized salt2. Pre-operative evaluation of each patient relied on history and physical examination, with screening for symptoms of thyroid dysfunction (specifically hyperthyroidism), anemia, and pregnancy. An excellent surgical nursing team ensured the two-bed operating rooms were properly prepared. We introduced our hospital’s time-out checklist, which we hope to formalize as a regular safety check in future surgeries performed at Kenyarelief.org. We worked side by side in a two-bed operating room, well stocked with equipment obtained through donations. All thyroid cases were performed with nerve monitoring and the aid of harmonic scissors. Given the limited access to medical care, performing total thyroidectomies, which would commit patients to lifelong daily medication, was not feasible. Thus, surgical planning focused on maintaining residual thyroid tissue to minimize the potential for hypothyroidism. Post-operatively, patients were monitored in the recovery room, often discharged the following day, trekking home on foot. Aside from visits to the clinic for suture removal, routine follow-up care including review of histopathology is currently unavailable. These limitations highlight important challenges and ethical considerations that still need to be overcome in the effort to provide safe care to our patients. At the completion of our three operative days, about 50 individuals were screened and 25 head and neck procedures performed, including 18 thyroidectomies for large goiters. Our experience, operatively and beyond, was inspiring. Our medical team, consisting of diverse medical personnel from across Kenya and the United States, shared a common mission and collaborated as though we had been operating together for years. Out of one week grew a fellowship with the local community, the orphans at Brittany’s Home, and our teammates that we hope will flourish with time. With a commitment to “never accept suffering,” we look forward to further collaboration to build on our efforts. With gratitude and appreciation to the AAO-HNSF Humanitarian Efforts Committee, Medtronic, Inc, and Ethicon, Inc for their generous support and donations. References UNICEF: The State of the World’s Children Report 2012. http://www.unicef.org/sowc2012 Adwok, John. Surgery in Africa—Monthly Review: Thyroid I: Endemic Surgery. 2006. http://www.ptolemy.ca/members/archives/2006/Endemic_Goiter.htm
Dunia Abdul-Aziz, MD
Harvard Otolaryngology Program
Boston, MA
The singing of children greeted us. After an eight-hour journey through the magnificent Rift Valley, we drove up to the gates of a walled compound in Migori, Kenya—a welcome sign to Brittany’s Home of Grace inviting us in.
In February, a team from the Massachusetts Eye and Ear Infirmary, Boston, composed of American Academy of Otolaryngology—Head and Neck Surgery members Gregory W. Randolph, MD; Paul Konowitz, MD; David J. Lesnik, MD; and myself, and surgical nurse Nancy Kotzuba, RN, joined nurses, anesthesiologists and local staff of KenyaRelief.org in a weeklong effort, with a goal of providing medical and surgical care to patients with head and neck disease, particularly goiters. The experience highlighted the power, the potential, and the challenges of international humanitarian initiatives.
This was our first time in Kenya, a country of about 39.4 million people, where the average income is slightly more than $2 a day1. We planned a thyroid mission to tackle endemic goiters, which remain prevalent despite salt iodization and Kenya’s status as the largest regional supplier of iodized salt2.
Pre-operative evaluation of each patient relied on history and physical examination, with screening for symptoms of thyroid dysfunction (specifically hyperthyroidism), anemia, and pregnancy. An excellent surgical nursing team ensured the two-bed operating rooms were properly prepared. We introduced our hospital’s time-out checklist, which we hope to formalize as a regular safety check in future surgeries performed at Kenyarelief.org.
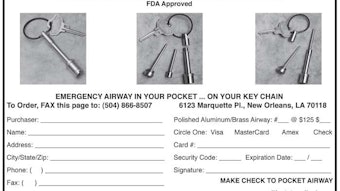
We worked side by side in a two-bed operating room, well stocked with equipment obtained through donations. All thyroid cases were performed with nerve monitoring and the aid of harmonic scissors. Given the limited access to medical care, performing total thyroidectomies, which would commit patients to lifelong daily medication, was not feasible. Thus, surgical planning focused on maintaining residual thyroid tissue to minimize the potential for hypothyroidism.
Post-operatively, patients were monitored in the recovery room, often discharged the following day, trekking home on foot. Aside from visits to the clinic for suture removal, routine follow-up care including review of histopathology is currently unavailable. These limitations highlight important challenges and ethical considerations that still need to be overcome in the effort to provide safe care to our patients.
At the completion of our three operative days, about 50 individuals were screened and 25 head and neck procedures performed, including 18 thyroidectomies for large goiters.
Our experience, operatively and beyond, was inspiring. Our medical team, consisting of diverse medical personnel from across Kenya and the United States, shared a common mission and collaborated as though we had been operating together for years. Out of one week grew a fellowship with the local community, the orphans at Brittany’s Home, and our teammates that we hope will flourish with time. With a commitment to “never accept suffering,” we look forward to further collaboration to build on our efforts.
With gratitude and appreciation to the AAO-HNSF Humanitarian Efforts Committee, Medtronic, Inc, and Ethicon, Inc for their generous support and donations.
References
- UNICEF: The State of the World’s Children Report 2012. http://www.unicef.org/sowc2012
- Adwok, John. Surgery in Africa—Monthly Review: Thyroid I: Endemic Surgery. 2006. http://www.ptolemy.ca/members/archives/2006/Endemic_Goiter.htm