The Academy Quality Agenda: Past, Present, and Future
Richard M. Rosenfeld, MD, MPH Senior Advisor for Guidelines and Quality During the past decade Academy leadership has quietly established a robust quality agenda, one that has positioned us as a leader in evidence-based medicine and clinical practice guideline development. We have reached a tipping point in our success, offering a unique opportunity to reflect on the past, appreciate the present, and to consider what the future might hold. Note: The comments that follow emphasize guidelines and measures, which are a key aspect of the quality agenda, but only part of the Academy’s diverse initiatives. Research and Health Policy The Tipping Point Author Malcolm Gladwell defines the tipping point as “the moment of critical mass, the threshold, the boiling point.” So what does this have to do with a quality agenda? Quite simply, we have reached the stage where the quality agenda has changed from an intellectual exercise to an eminently pragmatic—and essential—aspect of clinical practice that can empower otolaryngologists. Consider, for example, our ability to handle five significant external threats to physician autonomy because of our quality agenda: When the Joint Commission (JC) and American Medical Association (AMA) recently questioned the appropriateness of tympanostomy tube insertion in children we were able to rapidly mobilize a multidisciplinary guideline development group (including consumers), engage JC and AMA leadership in the process, and demonstrate our sincere commitment to addressing any quality concerns while preserving our member’s ability to perform necessary and appropriate surgery (2013 publication date). When WellPoint, home of the Anthem and Empire Blue Cross/Blue Shield insurance plans, began inappropriately denying tonsillectomy for children with sleep apnea or younger than age three with sleep-disordered breathing, we rapidly mobilized Academy Research and Health Policy leadership and used our quality products—guidelines on tonsillectomy and polysomnography—to achieve a prompt rewrite of the national WellPoint medical necessity policy with verbatim language proposed by the Academy. When the American Thyroid Association published a guideline on thyroid cancer that omitted any discussion of voice, laryngoscopy, or the recurrent laryngeal nerve, we created a multidisciplinary guideline emphasizing the role of laryngeal assessment and nerve monitoring in achieving optimal voice outcomes (2013 publication date). When the American Board of Internal Medicine Foundation asked specialty societies to identify, as part of their Choosing Wisely® campaign, “five tests or procedures commonly used in their field, whose necessity should be questioned and discussed,” we already had at our disposal numerous valid and actionable recommendations to choose from, based on our cadre of evidence-based clinical practice guidelines. When the AMA Physician Consortium on Performance Improvement (PCPI) sought to develop evidence-based measures for adult sinusitis and acute otitis externa, they enlisted otolaryngology leadership to co-chair the development process and used guidelines developed by our Academy as the basis for defining standards in the Physician Quality Reporting System. The Past Just a decade ago, none of the above would have been possible. Otolaryngologists did not have a seat at the national quality table and our Academy lacked the clout that would come only from an established and innovative quality program. Our response to the above concerns would largely have been symbolic, with a forced reliance on non-otolaryngology groups and organizations to defend our interests. Serious guideline development was perceived as something we ultimately “had to do,” but not necessarily what we would “want to do.” A false hope prevailed that clinical indicators, evidence-based reviews, and practice parameters would somehow create a quality mirage among stakeholders. With pay for performance (P4P) looming, it did not take long for this mirage to be replaced by a largely reactive acknowledgment that a serious quality program was sorely needed. The Present What a difference a decade makes. Our Academy has a thriving quality agenda and a state-of-the-art clinical practice guideline development program that has earned us not only a reserved seat at the national quality table, but also an international reputation for excellence. The Institute of Medicine and the Council for Medical Specialty Societies cited our guideline development manual, now in its third edition, as exemplifying best practice. Staff from our research, quality, and health policy business unit regularly teach, attend, and present at international venues. Our membership and staff are empowered through educational opportunities that include miniseminars, instructional courses, the Guideline Task Force, the Cochrane Scholars program, a new Guideline International Network (G-I-N) Scholars initiative, and hands-on participation and leadership training in guideline development groups. We have partnered with the Cochrane ENT Disorders Group for member training and systematic literature searches, and with the Yale Center for Medical Informatics in an AHRQ-funded project on guidelines and decision support. As practice assessment becomes an increasingly important aspect of maintenance of certification (part IV), Academy-developed guidelines are defining the clinical metrics for performance. The Future Our success with guideline development has laid the foundation for similar success in the related areas of dissemination, implementation, and knowledge transfer. We are also well equipped to internalize performance measure development, a task currently handled by the AMA-PCPI, but soon to be outsourced to medical specialty societies. Your Academy is well poised to develop quality products that promote best practice while preserving physician autonomy, which not only include multidisciplinary guidelines, but also encompass specialty-specific guidelines, clinical consensus statements, clinical indicators, and position (policy) statements. Efforts are under way to ensure our voice in the national dialogue integrating physician compensation with quality measures. We have grown from a timid and defensive player in the quality arena to a proactive Academy that will provide its members with quality tools and measures to meet the demands of diverse healthcare stakeholders. After a decade-long journey your Academy has emerged as a national quality leader, well ahead of many other professional medical societies, but with a limited portfolio of guidelines and measures. We now have the staff, processes, and leadership to forge ahead, but as a volunteer organization we cannot succeed without robust member engagement. There are many ways to get involved and have fun in the process. To express your interest and learn more about opportunities, please email Stephanie L. Jones, director of Research and Quality Improvement, at SLJones@entnet.org.
 Drs. Rosenfeld and Waguespock discuss with attendees the scope and detail of a guideline
Drs. Rosenfeld and Waguespock discuss with attendees the scope and detail of a guidelineRichard M. Rosenfeld, MD, MPH
Senior Advisor for Guidelines and Quality
During the past decade Academy leadership has quietly established a robust quality agenda, one that has positioned us as a leader in evidence-based medicine and clinical practice guideline development. We have reached a tipping point in our success, offering a unique opportunity to reflect on the past, appreciate the present, and to consider what the future might hold.
Note: The comments that follow emphasize guidelines and measures, which are a key aspect of the quality agenda, but only part of the Academy’s diverse initiatives.
Research and Health Policy The Tipping Point
Author Malcolm Gladwell defines the tipping point as “the moment of critical mass, the threshold, the boiling point.” So what does this have to do with a quality agenda? Quite simply, we have reached the stage where the quality agenda has changed from an intellectual exercise to an eminently pragmatic—and essential—aspect of clinical practice that can empower otolaryngologists.
Consider, for example, our ability to handle five significant external threats to physician autonomy because of our quality agenda:
- When the Joint Commission (JC) and American Medical Association (AMA) recently questioned the appropriateness of tympanostomy tube insertion in children we were able to rapidly mobilize a multidisciplinary guideline development group (including consumers), engage JC and AMA leadership in the process, and demonstrate our sincere commitment to addressing any quality concerns while preserving our member’s ability to perform necessary and appropriate surgery (2013 publication date).
- When WellPoint, home of the Anthem and Empire Blue Cross/Blue Shield insurance plans, began inappropriately denying tonsillectomy for children with sleep apnea or younger than age three with sleep-disordered breathing, we rapidly mobilized Academy Research and Health Policy leadership and used our quality products—guidelines on tonsillectomy and polysomnography—to achieve a prompt rewrite of the national WellPoint medical necessity policy with verbatim language proposed by the Academy.
- When the American Thyroid Association published a guideline on thyroid cancer that omitted any discussion of voice, laryngoscopy, or the recurrent laryngeal nerve, we created a multidisciplinary guideline emphasizing the role of laryngeal assessment and nerve monitoring in achieving optimal voice outcomes (2013 publication date).
- When the American Board of Internal Medicine Foundation asked specialty societies to identify, as part of their Choosing Wisely® campaign, “five tests or procedures commonly used in their field, whose necessity should be questioned and discussed,” we already had at our disposal numerous valid and actionable recommendations to choose from, based on our cadre of evidence-based clinical practice guidelines.
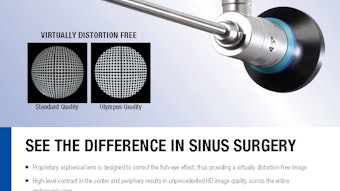
- When the AMA Physician Consortium on Performance Improvement (PCPI) sought to develop evidence-based measures for adult sinusitis and acute otitis externa, they enlisted otolaryngology leadership to co-chair the development process and used guidelines developed by our Academy as the basis for defining standards in the Physician Quality Reporting System.
The Past
Just a decade ago, none of the above would have been possible. Otolaryngologists did not have a seat at the national quality table and our Academy lacked the clout that would come only from an established and innovative quality program. Our response to the above concerns would largely have been symbolic, with a forced reliance on non-otolaryngology groups and organizations to defend our interests. Serious guideline development was perceived as something we ultimately “had to do,” but not necessarily what we would “want to do.” A false hope prevailed that clinical indicators, evidence-based reviews, and practice parameters would somehow create a quality mirage among stakeholders. With pay for performance (P4P) looming, it did not take long for this mirage to be replaced by a largely reactive acknowledgment that a serious quality program was sorely needed.
The Present
What a difference a decade makes. Our Academy has a thriving quality agenda and a state-of-the-art clinical practice guideline development program that has earned us not only a reserved seat at the national quality table, but also an international reputation for excellence. The Institute of Medicine and the Council for Medical Specialty Societies cited our guideline development manual, now in its third edition, as exemplifying best practice. Staff from our research, quality, and health policy business unit regularly teach, attend, and present at international venues.
Our membership and staff are empowered through educational opportunities that include miniseminars, instructional courses, the Guideline Task Force, the Cochrane Scholars program, a new Guideline International Network (G-I-N) Scholars initiative, and hands-on participation and leadership training in guideline development groups. We have partnered with the Cochrane ENT Disorders Group for member training and systematic literature searches, and with the Yale Center for Medical Informatics in an AHRQ-funded project on guidelines and decision support. As practice assessment becomes an increasingly important aspect of maintenance of certification (part IV), Academy-developed guidelines are defining the clinical metrics for performance.
The Future
Our success with guideline development has laid the foundation for similar success in the related areas of dissemination, implementation, and knowledge transfer. We are also well equipped to internalize performance measure development, a task currently handled by the AMA-PCPI, but soon to be outsourced to medical specialty societies.
Your Academy is well poised to develop quality products that promote best practice while preserving physician autonomy, which not only include multidisciplinary guidelines, but also encompass specialty-specific guidelines, clinical consensus statements, clinical indicators, and position (policy) statements. Efforts are under way to ensure our voice in the national dialogue integrating physician compensation with quality measures.
We have grown from a timid and defensive player in the quality arena to a proactive Academy that will provide its members with quality tools and measures to meet the demands of diverse healthcare stakeholders.
After a decade-long journey your Academy has emerged as a national quality leader, well ahead of many other professional medical societies, but with a limited portfolio of guidelines and measures. We now have the staff, processes, and leadership to forge ahead, but as a volunteer organization we cannot succeed without robust member engagement. There are many ways to get involved and have fun in the process. To express your interest and learn more about opportunities, please email Stephanie L. Jones, director of Research and Quality Improvement, at SLJones@entnet.org.