Clinical Practice Guidelines: Resources for Optimizing “Kids E.N.T.” Practice
Kathleen Billings, MD Assistant Professor, Division of Otolaryngology-Head and Neck Surgery Ann and Robert H. Lurie Children’s Hospital of Chicago David E. Tunkel, MD Director of Pediatric Otolaryngology Johns Hopkins Medical Institutions Clinical practice guidelines (CPGs) are excellent resources that bring evidence-based medicine to practicing clinicians and patients. A CPG, as noted by the Institute of Medicine (IOM), contains “statements that include recommendations intended to optimize patient care that are informed by systematic review of the evidence and an assessment of the benefits and harms of alternative care options.”1 CPGs summarize available evidence about specific clinical conditions, treatments, and procedures to help promote best practices with the use of action statements. They also identify areas for future research where evidence may be lacking. The American Academy of Otolaryngology—Head and Neck Surgery Foundation (AAO-HNSF) has been a leader in CPG development since 2006, using experts in the field of otolaryngology, methodologists, experienced staff liaisons, allied health professionals, and selected additional stakeholders to create CPGs and clinical consensus statements. Recent CPGs address important aspects of otolaryngologic care for children. The Guideline Development Taskforce (GDTF), first chaired by Richard M. Rosenfeld MD, MPH, and now by Seth R. Schwartz, MD, MPH, solicits, evaluates, and prioritizes topics for CPGs or clinical consensus statements. AAO-HNS/F committees, subspecialty societies, and even individual Academy Members can advance proposals for CPGs. CPGs have been published about management of cerumen impaction and acute otitis externa, topics certainly relevant to care of children with ear disease.2,3 More recently, “Clinical Practice Guidelines for Tonsillectomy in Children,” and “The Use of Polysomnography (PSG) for Sleep-disordered Breathing Prior to Tonsillectomy in Children” were published.4,5 The tonsillectomy guideline emphasizes appropriate indications for children with recurrent throat infection and sleep-disordered breathing. Other key action statements present recommendations and supporting evidence about perioperative care for children undergoing tonsillectomy, including the use of antibiotics, steroids, and analgesics. The action statements in the PSG guideline provide guidance for selection of children who benefit most from a PSG before tonsillectomy, and present indications for overnight monitoring after surgery for children with obstructive sleep disorders. CPGs relevant to otolaryngology care have been developed by many organizations worldwide. In fact, the National Guideline Clearinghouse currently lists 81 guidelines under the search term “otorhinolaryngology” on its website, guidelines.gov, and many of these involve pediatric care issues. The IOM has emphasized the need for trustworthy CPGs, with recommendations for transparency in the development process, management of conflicts of interest, and inclusion of a broad group of stakeholders.1 The AAO-HNSF guideline task forces use a defined methodology to produce reliable guidelines with actionable statements. While the development process has been published in detail, key components of the process include a systematic evaluation of the available evidence in the literature, involvement of a broad group of stakeholders from multiple disciplines, an external review process, and a public comment period.6 The treatment of otitis media in children is the subject of two soon-to-be completed CPGs. The American Academy of Pediatrics (AAP) published a CPG for “Diagnosis and Management of Acute Otitis Media (AOM),” in 2004.7 Statements in this CPG advanced the concept of initial management without antibiotics for children older than two years of age without severe disease. This AOM guideline has been updated by a committee of the AAP, and is scheduled for publication in early 2013. The observation option for children with AOM will be refined, based on results of recent clinical trials, and tympanostomy tubes are considered an option for prevention of AOM in otitis media-prone children. The AAO-HNSF CPG on tympanostomy tubes in children is completing review, with publication expected during 2013. This CPG is timely, as tympanostomy tubes have been identified as an overused procedure, particularly for healthy children with short-term middle ear effusions. The tympanostomy tube CPG will discuss surgical indications for children with long-term effusions, and will provide action statements to guide surgical decision-making for children with recurrent AOM. The importance of identifying children who are at risk for developmental consequences of persistent OME will be emphasized. Several action statements will address care issues for children with indwelling tubes. Clinical consensus statements have also been developed for topics where high-level evidence does not exist to allow a full CPG, but where consensus can be developed to reduce variation in practices and improve care. A consensus statement about “Appropriate Use of Computed Tomography for Paranasal Sinus Disease,” was published in November 2012.8 Specific recommendations were made about timing and selection of imaging for children with sinus disease. This document may help reduce unnecessary exposure of children to ionizing radiation. A consensus statement on tracheostomy care was published in January of this year, and eight statements about children with tracheostomy are included.9 We look forward to a pediatric chronic rhinosinusitis consensus statement that has been approved for development by the GDTF. We must emphasize that a CPG is not a substitute for clinical judgment and does not serve as a protocol for all patients and clinical situations.10 Healthcare providers and patients must be educated about CPGs, as awareness and adoption are as important as the development process. Finally, as healthcare advances and practices change, the CPGs must be revisited and perhaps revised to provide up-to-date optimal treatment. Additional information about clinical practice guideline development by the AAO-HNSF can be found at entnet.org/Practice/clinicalPracticeguidelines.cfm and www.entnet.org/Practice/upload/GDTF-Summer-2012-Newsletter_Final.pdf. References Institute of Medicine. Clinical practice guidelines we can trust. Consensus report. March 23, 2011. Roland PS, Smith TL, Schwartz SR, Rosenfeld RM, et al. Clinical practice guideline: cerumen impaction. Otolaryngol Head Neck Surg. 2008; 139:S1-48. Rosenfeld RM, Brown L, Cannon CR, Dolor RJ, et al. Clinical practice guideline: acute otitis externa. Otolaryngol Head Neck Surg. 2006; 134:S4-23. Baugh RF, Archer SF, Mitchell RB, Rosenfeld RM, et al. Clinical practice guideline: tonsillectomy in children. Otolaryngol Head Neck Surg. 2011; 144:S1-30. Roland PS, Rosenfeld RM, Brooks LJ, Friedman NR, et al. Clinical practice guideline: polysomnography for sleep-disordered breathing prior to tonsillectomy in children. Otolaryngol Head Neck Surg. 2011; 145:S1-15. Rosenfeld RM, Shiffman RN, Robertson P. Clinical practice guideline development manual, third edition: a quality-driven approach for translating evidence into action. Otolaryngol Head and Neck. Jan 2013; 148 (1 Suppl):S1-S55. AAP Committee on Acute Otitis Media. Diagnosis and management of acute otitis media. Pediatrics. 2004; 113:1451-1465. Setzen G, Ferguson BJ, Han JK, Rhee JS, et al. Clinical consensus statement: appropriate use of computed tomography for paranasal sinus disease. Otolaryngol Head Neck Surg. 2012: 147:808-816. Mitchell RB, Hussey HM, Setzen G, Jacobs IN, et al. Clinical consensus statement: tracheotomy care. Otolaryngol Head Neck Surg. 2012; published online 18 September 2012. Rosenfeld RM. Guidelines and otolaryngology. Otolaryngol Head Neck Surg. 2006; 134:S1-3. Social Media for Kids E.N.T. Health MonthThe Academy plans to post the following messages on our social media sites. Share with your patients and add your own. 1. February is Kids E.N.T. Month, learn more: www.entnet.org/AboutUs/kidsENT.cfm 2. Learn more about Choking Hazards in children: www.entnet.org/AboutUs/kidsENT.cfm 3. Choking Hazards Campaign audio is now live, visit http://www.entnet.org/HealthInformation/Choking-Campaign.cfm for more information! 4. Share this information with your practice and the public by utilizing our draft template, learn more: www.entnet.org/AboutUs/kidsENT.cfm 5. Visit our Kids E.N.T. Health Library http://www.entnet.org/HealthInformation/pediatric.cfm 6. What to Expect after Your Child Has Tonsillectomy/Adenoidectomy Surgery: http://www.entnet.org/AboutUs/upload/Post-t-a-fact-sheet.pdf 7. Check out the Button Battery article in the February issue of the Bulletin (to be posted via social media) 8. See a re-post of this Bulletin article on Kids E.N.T. health online at: www.entnet.org/bulletin
Kathleen Billings, MD
Assistant Professor, Division of
Otolaryngology-Head and Neck Surgery
Ann and Robert H. Lurie Children’s Hospital of Chicago
David E. Tunkel, MD
Director of Pediatric Otolaryngology
Johns Hopkins Medical Institutions
Clinical practice guidelines (CPGs) are excellent resources that bring evidence-based medicine to practicing clinicians and patients. A CPG, as noted by the Institute of Medicine (IOM), contains “statements that include recommendations intended to optimize patient care that are informed by systematic review of the evidence and an assessment of the benefits and harms of alternative care options.”1 CPGs summarize available evidence about specific clinical conditions, treatments, and procedures to help promote best practices with the use of action statements. They also identify areas for future research where evidence may be lacking.
The American Academy of Otolaryngology—Head and Neck Surgery Foundation (AAO-HNSF) has been a leader in CPG development since 2006, using experts in the field of otolaryngology, methodologists, experienced staff liaisons, allied health professionals, and selected additional stakeholders to create CPGs and clinical consensus statements. Recent CPGs address important aspects of otolaryngologic care for children.
The Guideline Development Taskforce (GDTF), first chaired by Richard M. Rosenfeld MD, MPH, and now by Seth R. Schwartz, MD, MPH, solicits, evaluates, and prioritizes topics for CPGs or clinical consensus statements. AAO-HNS/F committees, subspecialty societies, and even individual Academy Members can advance proposals for CPGs. CPGs have been published about management of cerumen impaction and acute otitis externa, topics certainly relevant to care of children with ear disease.2,3 More recently, “Clinical Practice Guidelines for Tonsillectomy in Children,” and “The Use of Polysomnography (PSG) for Sleep-disordered Breathing Prior to Tonsillectomy in Children” were published.4,5 The tonsillectomy guideline emphasizes appropriate indications for children with recurrent throat infection and sleep-disordered breathing. Other key action statements present recommendations and supporting evidence about perioperative care for children undergoing tonsillectomy, including the use of antibiotics, steroids, and analgesics. The action statements in the PSG guideline provide guidance for selection of children who benefit most from a PSG before tonsillectomy, and present indications for overnight monitoring after surgery for children with obstructive sleep disorders.
CPGs relevant to otolaryngology care have been developed by many organizations worldwide. In fact, the National Guideline Clearinghouse currently lists 81 guidelines under the search term “otorhinolaryngology” on its website, guidelines.gov, and many of these involve pediatric care issues. The IOM has emphasized the need for trustworthy CPGs, with recommendations for transparency in the development process, management of conflicts of interest, and inclusion of a broad group of stakeholders.1
The AAO-HNSF guideline task forces use a defined methodology to produce reliable guidelines with actionable statements. While the development process has been published in detail, key components of the process include a systematic evaluation of the available evidence in the literature, involvement of a broad group of stakeholders from multiple disciplines, an external review process, and a public comment period.6
The treatment of otitis media in children is the subject of two soon-to-be completed CPGs. The American Academy of Pediatrics (AAP) published a CPG for “Diagnosis and Management of Acute Otitis Media (AOM),” in 2004.7 Statements in this CPG advanced the concept of initial management without antibiotics for children older than two years of age without severe disease. This AOM guideline has been updated by a committee of the AAP, and is scheduled for publication in early 2013. The observation option for children with AOM will be refined, based on results of recent clinical trials, and tympanostomy tubes are considered an option for prevention of AOM in otitis media-prone children.
The AAO-HNSF CPG on tympanostomy tubes in children is completing review, with publication expected during 2013. This CPG is timely, as tympanostomy tubes have been identified as an overused procedure, particularly for healthy children with short-term middle ear effusions. The tympanostomy tube CPG will discuss surgical indications for children with long-term effusions, and will provide action statements to guide surgical decision-making for children with recurrent AOM. The importance of identifying children who are at risk for developmental consequences of persistent OME will be emphasized. Several action statements will address care issues for children with indwelling tubes.
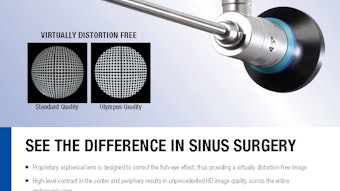
Clinical consensus statements have also been developed for topics where high-level evidence does not exist to allow a full CPG, but where consensus can be developed to reduce variation in practices and improve care. A consensus statement about “Appropriate Use of Computed Tomography for Paranasal Sinus Disease,” was published in November 2012.8 Specific recommendations were made about timing and selection of imaging for children with sinus disease. This document may help reduce unnecessary exposure of children to ionizing radiation. A consensus statement on tracheostomy care was published in January of this year, and eight statements about children with tracheostomy are included.9 We look forward to a pediatric chronic rhinosinusitis consensus statement that has been approved for development by the GDTF.
We must emphasize that a CPG is not a substitute for clinical judgment and does not serve as a protocol for all patients and clinical situations.10 Healthcare providers and patients must be educated about CPGs, as awareness and adoption are as important as the development process. Finally, as healthcare advances and practices change, the CPGs must be revisited and perhaps revised to provide up-to-date optimal treatment. Additional information about clinical practice guideline development by the AAO-HNSF can be found at entnet.org/Practice/clinicalPracticeguidelines.cfm and www.entnet.org/Practice/upload/GDTF-Summer-2012-Newsletter_Final.pdf.
References
- Institute of Medicine. Clinical practice guidelines we can trust. Consensus report. March 23, 2011.
- Roland PS, Smith TL, Schwartz SR, Rosenfeld RM, et al. Clinical practice guideline: cerumen impaction. Otolaryngol Head Neck Surg. 2008; 139:S1-48.
- Rosenfeld RM, Brown L, Cannon CR, Dolor RJ, et al. Clinical practice guideline: acute otitis externa. Otolaryngol Head Neck Surg. 2006; 134:S4-23.
- Baugh RF, Archer SF, Mitchell RB, Rosenfeld RM, et al. Clinical practice guideline: tonsillectomy in children. Otolaryngol Head Neck Surg. 2011; 144:S1-30.
- Roland PS, Rosenfeld RM, Brooks LJ, Friedman NR, et al. Clinical practice guideline: polysomnography for sleep-disordered breathing prior to tonsillectomy in children. Otolaryngol Head Neck Surg. 2011; 145:S1-15.
- Rosenfeld RM, Shiffman RN, Robertson P. Clinical practice guideline development manual, third edition: a quality-driven approach for translating evidence into action. Otolaryngol Head and Neck. Jan 2013; 148 (1 Suppl):S1-S55.
- AAP Committee on Acute Otitis Media. Diagnosis and management of acute otitis media. Pediatrics. 2004; 113:1451-1465.
- Setzen G, Ferguson BJ, Han JK, Rhee JS, et al. Clinical consensus statement: appropriate use of computed tomography for paranasal sinus disease. Otolaryngol Head Neck Surg. 2012: 147:808-816.
- Mitchell RB, Hussey HM, Setzen G, Jacobs IN, et al. Clinical consensus statement: tracheotomy care. Otolaryngol Head Neck Surg. 2012; published online 18 September 2012.
- Rosenfeld RM. Guidelines and otolaryngology. Otolaryngol Head Neck Surg. 2006; 134:S1-3.
1. February is Kids E.N.T. Month, learn more: www.entnet.org/AboutUs/kidsENT.cfm
2. Learn more about Choking Hazards in children: www.entnet.org/AboutUs/kidsENT.cfm
3. Choking Hazards Campaign audio is now live, visit http://www.entnet.org/HealthInformation/Choking-Campaign.cfm for more information!
4. Share this information with your practice and the public by utilizing our draft template, learn more: www.entnet.org/AboutUs/kidsENT.cfm
5. Visit our Kids E.N.T. Health Library http://www.entnet.org/HealthInformation/pediatric.cfm
6. What to Expect after Your Child Has Tonsillectomy/Adenoidectomy Surgery: http://www.entnet.org/AboutUs/upload/Post-t-a-fact-sheet.pdf
7. Check out the Button Battery article in the February issue of the Bulletin (to be posted via social media)
8. See a re-post of this Bulletin article on Kids E.N.T. health online at: www.entnet.org/bulletin