Developing Facial Plastic and Reconstructive Surgery Modules for the OCC
The newly launched modules within the Otolaryngology Core Curriculum (OCC) aim to standardize and elevate training in this diverse subspecialty.
James C. Wang, MD, PhD, member, Facial Plastic and Reconstructive Surgery Education Committee
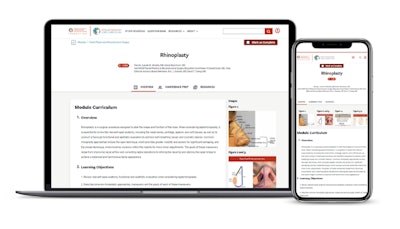
Facial plastic and reconstructive surgery (FPRS) is a critical subspecialty within otolaryngology-head and neck surgery, addressing a wide range of conditions from aesthetics (e.g., rhinoplasty, rhytidectomies, blepharoplasties, and injectables) to congenital anomalies (e.g., cleft lip and palate, microtia) to facial reconstruction (e.g., cutaneous, trauma, and acquired facial deformities). Various education resources are available to otolaryngologists and trainees, but a succinct repository of peer-reviewed, high-yield information for the subspecialty was lacking1-4 before the Otolaryngology Core Curriculum (OCC) was launched in July 2024.
When I went through my training, various resources were available as large-format textbooks (e.g., Cummings, Baileys, Papel), study guides (e.g., Michael Cunningham’s Otolaryngology-Prep and Practice, K.J. Lee’s Essential Otolaryngology, and Frank Lin’s ENT Board Prep) pocket guides (e.g. Pasha’s Otolaryngology, Desai’s Facial Plastic and Reconstructive Surgery), and question banks (e.g., BoardVitals, OTO Quest, and StatPearls). Notably, these question banks, aside from the AAO-HNSF OTO Quest – Knowledge Assessment Tool, are not vetted by otolaryngologists, and the knowledge contained is not necessarily applicable to board examinations or clinical practice.
The training experience for FPRS varies significantly among institutions, leading to inconsistencies in resident knowledge and skills. For instance, only certain programs have exposure to cleft lip and palate repair as well as facial feminization procedures. In addition, the exposure to facial resurfacing using chemical peels versus lasers varies considerably. As for other subspecialties of otolaryngology, a single, unified curriculum was needed to help standardize training in FPRS. In addition to standardizing training, the OCC aims to fulfill several key objectives, including enhancing clinical competency and allowing round table discussions of key topics.
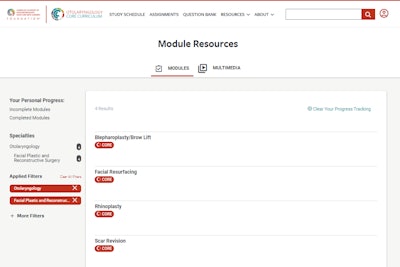
The OCC officially launched on July 1, 2024, with the 25 Phase 1 modules, including FPRS modules “rhinoplasty,” blepharoplasty/brow lift,” and “scar revision/resurfacing.” The FPRS modules are aimed at enhancing education for resident physicians and addressing disparities by ensuring all residents acquire essential competencies in facial plastic and reconstructive surgery, regardless of their training program.5 The second phase of modules is set to debut on January 1, 2025, and includes topics such as cutaneous facial reconstruction and reanimation.
Implementing a standardized curriculum presents its own challenges. There is a significant cost to develop, publish, and maintain the curriculum, which is supported by a subscription fee for each U.S.-based institution using the curriculum. As of October 2024, 83% of the otolaryngology-head and neck surgery residency programs in the United States have subscribed to the OCC. Further research based on Otolaryngology Training Exam (in-service) scores will help delineate if this curriculum has had a positive impact on resident education. Access to the OCC for private practice physicians, advanced practice providers, and international trainees and physicians will be rolled out over the coming year.
The development of a core curriculum in FPRS serves to unify the high-yield information needed to train otolaryngology head and neck surgery residents by establishing a structured approach to training based on evidence-based practices.
References
- Snyderman, C. H., et al. (2018). Global Perspectives in Facial Plastic Surgery Education. Facial Plastic Surgery Clinics of North America, 26(4), 401-410.
- Klein, A., Gupta, S., & Vyas, R. (2019). Essential Knowledge in Facial Plastic Surgery: Curriculum Development and Implementation. JAMA Facial Plastic Surgery, 21(5), 365-370.
- Harris, R. J., et al. (2021). Simulation-Based Learning in Facial Plastic Surgery: Bridging the Gap in Education. Plastic and Reconstructive Surgery, 147(4), 876-884.
- Brown, T., et al. (2022). Challenges in Implementing Global Surgical Education Programs. Annals of Surgery, 275(3), 589-597.
- Wang, D., Lee, C., & Williams, K. (2020). Standardizing Facial Plastic Surgery Education: A Call to Action. Otolaryngology Clinics of North America, 53(2), 123-135.