Expanding Cleft and Craniofacial Education through Virtual Simulation
Learn how virtual simulation is transforming cleft and craniofacial surgical training, offering global access to invaluable expert-led, hands-on practice.
Brianne Barnett Roby, MD, and Alexander P. Marston, MD, on behalf of the Otolaryngology Cleft and Craniofacial Committee

The committee has undertaken this important task to educate all Academy members on standardizing care for children and adults with cleft and craniofacial differences. Education offerings thus far have included not only podcasts, webinars, panels, and videos but also a unique simulation education program for residents and fellows who may not have exposure to these types of surgical procedures.
Launch of Cleft and Craniofacial Bootcamp

Expanded Virtual Simulation Training
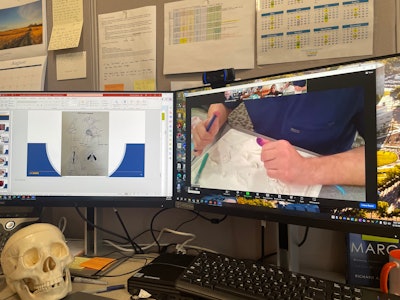
Delivering effective, simultaneous virtual training for participants and faculty located around the world requires collaborative planning and synchronized execution. Before the simulation event, high-fidelity cleft lip and cleft palate 3D simulator models fabricated with silicone and polylactic acid,1 as well as 3D costal cartilage silicone material (makemedical™) are mailed to the participants. Additionally, a document is emailed to each fellow with surgical technique instructions and pre- and post-simulation surveys. Each fellow is responsible for borrowing the necessary surgical instruments from their sponsoring medical center. A basic cutting board is recommended when carving the silicone materials to create the microtia construct and rhinoplasty grafts.
Real-Time Virtual Training and Feedback

The sessions are executed according to a series of advancing objectives. The cleft lip simulation module handbook instructions suggest a rotation-advancement Millard-type repair technique, while the cleft palate simulation suggests a Furlow palatoplasty technique. The microtia simulation directs each fellow to practice carving the base framework, helical rim, antihelix, incisura, and tragus. Sutures are then used to assemble the microtia construct. Participants are in each virtual “room” for 45 minutes. After the simulation, the fellows complete the post-survey to assess the knowledge they acquired and to further improve the curriculum and training.
Cleft lip and palate repair, microtia reconstruction, and rhinoplasty all require a high level of expertise and experience to achieve a desirable post-operative result. As a result, this virtual simulation offers the participants unique and important opportunities to practice and conceptualize complex, multistep cleft repairs and graft carving with the virtual guidance of experts in the field. In 2024, participants included 37 pediatric fellows, 11 facial plastic and reconstructive surgery fellows, and 12 international fellows along with 16 faculty members.
A Platform for Learning and Skill Development
The committee is committed to providing a safe space to learn and practice procedures that may be less accessible in many training programs. Looking ahead, the committee believes simulation will continue to advance education for complex cleft and craniofacial procedures. For the broader Academy membership, webinars and podcasts on topics like managing nasal obstruction, eustachian tube dysfunction, and obstructive sleep apnea in cleft and craniofacial patients should help general otolaryngologists to build confidence in managing these common issues within a complex patient population. The Otolaryngology Cleft and Craniofacial Committee remains passionately dedicated to sharing valuable resources and knowledge with all otolaryngology-head and neck surgeons worldwide.
Reference
- Reighard CL, Green K, Rooney DM, Zopf DA. Development of a Novel, Low-Cost, High-fidelity Cleft Lip Repair Surgical Simulator Using Computer-Aided Design and 3-Dimensional Printing. JAMA Facial Plast Surg. 2019;21:77-79.