Value-Based Modifier Program: How Will It Affect You?
The Value-Based Modifier (VBM) Program assesses both quality of care furnished and the cost of care under the Medicare Physician Fee Schedule (MPFS). The Centers for Medicare & Medicaid Services (CMS) are beginning with a phase-in of the VBM in 2015, which will apply to all physicians by January 1, 2017. Implementation of the VBM is based on participation in Physician Quality Reporting System (PQRS). For CY 2013, the VBM applied to groups of physicians with 100 or more eligible professionals (EPs). In 2014, CMS is expanding this to groups with 10 or more. Groups are defined, for purposes of the VBM, as “a physician (includes doctors of medicine or osteopathy, doctors of dental surgery or dental medicine, doctors of podiatric medicine, doctors of optometry, and chiropractors); OR a practitioner described as (a physical or occupational therapist or qualified SLP; or a qualified audiologist).” To determine what groups have more than 10 providers for purposes of the 2014 VBM reporting period, CMS will query their PECOS system to identify groups and will perform the query 10 days after the close of the PQRS group self-nomination/registration process which occurs in the fall of the year prior to the upcoming reporting period (i.e. occurred in October 2013 for CY 2014 PQRS reporting period). Of note, CMS will not apply the VBM to groups of physicians that are participating in the MSSP program, the Pioneer ACO models, or the Comprehensive Primary Care initiative. Physician Quality Resource Use Reports Eligible professionals (EPs) are able to assess their performance, and how they would have performed had the VBM been applied to them in 2013, by downloading their Quality Resource Use Reports (QRURs) from the CMS website at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeedbackProgram/Episode-Costs-and-Medicare-Episode-Grouper.html. These reports will inform physicians how they compare in cost and quality of care to their peers. Visit the Academy website for specifics on obtaining your report at http://bit.ly/entVBPM. Each group then receives two composite scores (quality and cost), based on the group’s standardized performance (e.g., how far away from the national mean). Group cost measures are adjusted for specialty composition of the group. This approach identifies statistically significant outliers and assigns them to their respective quality and cost tiers. Attribution of Beneficiaries for Purposes of Assigning Costs CMS will use the same methodology used for the MSSP ACO program to assign beneficiaries to groups for purposes of the VBM. That is, they will assign beneficiaries based on the delivery of primary care services. For groups that do not provide primary care services, or who have fewer than 20 beneficiaries attributed to them, CMS will assign their cost composite as “average” cost. For the new 2014 cost measure on Medicare Spending Per Beneficiary (see chart), CMS will attribute the Medicare spending per beneficiary (MSPB) episode solely to the physician group, identified by the TIN, that provided the plurality of Part B services billed during the index hospitalization. CMS will also require physicians to have a minimum of MSPB episodes attributed to them before this measure would be included in their cost composite for calculation of the VBM. Cost Composites and Benchmarking CMS will account for specialty mix using a “specialty adjustment” method as it relates to calculating a group’s standardized score for each cost measure and benchmarking against other groups for that performance year. The new specialty adjustment will entail the following: Creating a national specialty-specific expected costs; Calculating a specialty-adjusted expected cost for each group of physicians by weighing the national specialty-specific expected costs by the group’s specialty composition of Part B payments; and Calculating a specialty-adjusted total per capita cost. CMS will identify the specialty for each EP based on the specialty they have listed on the largest share of their Part B claims. CMS states that the “specialty adjustment” method accounts for the specialty composition of the group of physicians when making peer group comparisons and creates standardized scores for each cost measure. They also believe this methodology allows the payment modifier to apply to smaller size groups and solo practitioners. CMS states that although the calculations are very detailed, they are transparent and they can provide each group of physicians information on how their costs were benchmarked. CMS believes that the “comparability peer group” method would be less transparent. CMS does not believe it is necessary to delay implementation and will monitor the influence of the specialty adjustment method on physician groups. Specifics on 2014 VBM requirements are outlined and additional information is available on the Academy website, including a new VBM Fact Sheet, at http://bit.ly/entVBPM. How Does the Value Modifier Work with PQRS? How are My Quality and Cost Scores Calculated?
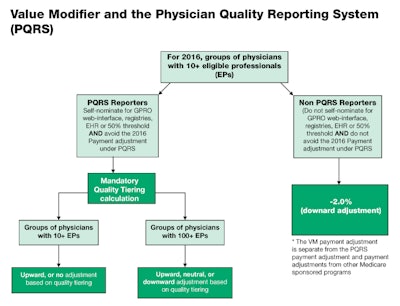
The Value-Based Modifier (VBM) Program assesses both quality of care furnished and the cost of care under the Medicare Physician Fee Schedule (MPFS). The Centers for Medicare & Medicaid Services (CMS) are beginning with a phase-in of the VBM in 2015, which will apply to all physicians by January 1, 2017. Implementation of the VBM is based on participation in Physician Quality Reporting System (PQRS). For CY 2013, the VBM applied to groups of physicians with 100 or more eligible professionals (EPs). In 2014, CMS is expanding this to groups with 10 or more.
Groups are defined, for purposes of the VBM, as “a physician (includes doctors of medicine or osteopathy, doctors of dental surgery or dental medicine, doctors of podiatric medicine, doctors of optometry, and chiropractors); OR a practitioner described as (a physical or occupational therapist or qualified SLP; or a qualified audiologist).” To determine what groups have more than 10 providers for purposes of the 2014 VBM reporting period, CMS will query their PECOS system to identify groups and will perform the query 10 days after the close of the PQRS group self-nomination/registration process which occurs in the fall of the year prior to the upcoming reporting period (i.e. occurred in October 2013 for CY 2014 PQRS reporting period). Of note, CMS will not apply the VBM to groups of physicians that are participating in the MSSP program, the Pioneer ACO models, or the Comprehensive Primary Care initiative.
Physician Quality Resource Use Reports
Eligible professionals (EPs) are able to assess their performance, and how they would have performed had the VBM been applied to them in 2013, by downloading their Quality Resource Use Reports (QRURs) from the CMS website at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeedbackProgram/Episode-Costs-and-Medicare-Episode-Grouper.html. These reports will inform physicians how they compare in cost and quality of care to their peers. Visit the Academy website for specifics on obtaining your report at http://bit.ly/entVBPM.
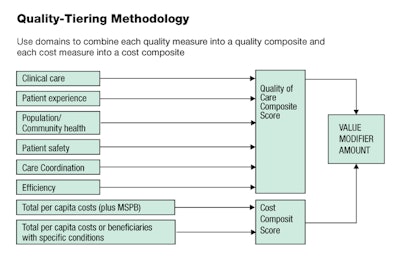
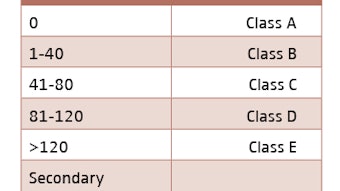
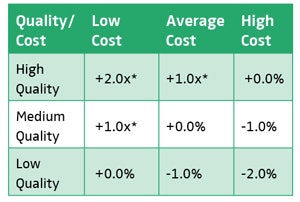
Each group then receives two composite scores (quality and cost), based on the group’s standardized performance (e.g., how far away from the national mean). Group cost measures are adjusted for specialty composition of the group. This approach identifies statistically significant outliers and assigns them to their respective quality and cost tiers.
Attribution of Beneficiaries for Purposes of Assigning Costs
CMS will use the same methodology used for the MSSP ACO program to assign beneficiaries to groups for purposes of the VBM. That is, they will assign beneficiaries based on the delivery of primary care services. For groups that do not provide primary care services, or who have fewer than 20 beneficiaries attributed to them, CMS will assign their cost composite as “average” cost.
For the new 2014 cost measure on Medicare Spending Per Beneficiary (see chart), CMS will attribute the Medicare spending per beneficiary (MSPB) episode solely to the physician group, identified by the TIN, that provided the plurality of Part B services billed during the index hospitalization. CMS will also require physicians to have a minimum of MSPB episodes attributed to them before this measure would be included in their cost composite for calculation of the VBM.
Cost Composites and Benchmarking
CMS will account for specialty mix using a “specialty adjustment” method as it relates to calculating a group’s standardized score for each cost measure and benchmarking against other groups for that performance year. The new specialty adjustment will entail the following:
- Creating a national specialty-specific expected costs;
- Calculating a specialty-adjusted expected
cost for each group of physicians by weighing the national specialty-specific expected costs by the group’s specialty composition of Part B payments; and - Calculating a specialty-adjusted total per capita cost.
CMS will identify the specialty for each EP based on the specialty they have listed on the largest share of their Part B claims. CMS states that the “specialty adjustment” method accounts for the specialty composition of the group of physicians when making peer group comparisons and creates standardized scores for each cost measure. They also believe this methodology allows the payment modifier to apply to smaller size groups and solo practitioners. CMS states that although the calculations are very detailed, they are transparent and they can provide each group of physicians information on how their costs were benchmarked. CMS believes that the “comparability peer group” method would be less transparent. CMS does not believe it is necessary to delay implementation and will monitor the influence of the specialty adjustment method on physician groups.
Specifics on 2014 VBM requirements are outlined and additional information is available on the Academy website, including a new VBM Fact Sheet, at http://bit.ly/entVBPM.
How Does the Value Modifier Work with PQRS?
How are My Quality and Cost Scores Calculated?