Out of Committee: Hearing and Equilibrium Standards for the Diagnosis and Evaluation of Therapy in Meniere’s Disease
Communication from the Committee on Equilibrium The 1995 Committee on Hearing and Equilibrium Guidelines for the Diagnosis and Evaluation of Therapy in Meniere’s Disease established a practical and useful framework for the reporting of results in Meniere’s treatment and outcomes research, by comparing the frequency of definite attacks for the period six months before treatment compared with the interval occurring between 18 and 24 months after treatment (ref1). Class A-F results were defined, based on a comparison of the frequency of spells (see Table 1). Class F outcome was reported if secondary treatment was initiated due to disability from vertigo. As Meniere’s disease has evolved from a “disease” to Meniere’s syndrome, and as treatment options have changed since the initial publication in 1995, the Committee on Equilibrium has prepared this document to serve as an assessment and publication standard for current and future reporting on Meniere’s syndrome. With the advent of intratympanic therapy for Meniere’s syndrome, the accurate application of the prior guidelines to reports including intratympanic therapy as a treatment was impossible, since intratympanic therapy is often performed repeatedly, dependent on symptom severity. As such, the committee suggests considering intratympanic therapies as “intent to treat” events. The patient would enter the “intratympanic steroid treatment” or “intratympanic gentamicin treatment” arm, and irrespective of the number of treatments, outcome at 18 months to 24 months could be compared to other treatments, such as medical management or surgery. Progression to a secondary treatment other than the original “intent to treat” arm would still be considered a class F event. Patients in the “intratympanic steroid intent to treat” arm would be classified as class F if they entered the “intratympanic gentamicin intent to treat” arm. The frequency of intratympanic treatment could also be reported in any publication, and would add additional relevant detail to the evaluation of this treatment. The committee considered whether outcome reporting based totally on frequency of attacks was an optimal strategy. The current A-F reporting guidelines are based solely on frequency of attacks, are in wide use, and have been a standard of comparability in the literature. However, more information regarding the severity of attacks would be useful in evaluating therapies. The committee recommended the following five-point scale of daily vertigo severity, with acknowledgement that other daily vertigo severity scales are also in use: 0—No vertigo. 1—Mild attack—brief episode of vertigo lasting less than 20 minutes and/or vague sense of disequilibrium lasting less than two hours. 2—Moderate attack—vertigo lasting between 20 to 60 minutes and/or disequilibrium lasting greater than two hours with reduction in daily activities from 0 percent to 50 percent. 3—Severe attack—vertigo lasting more than one hour with or without accompanying nausea and vomiting, with or without lingering disequilibrium lasting greater than two hours with reduction in daily activities. between 50 percent to 100 percent. 4—Extreme attack—vertigo lasting more than one hour with nausea and vomiting and persistent lingering severe disequilibrium requiring bed rest the entire day. The numerical value is the ratio of the average number of vertigo spells during the pretreatment period divided by the average number of vertigo spells for the same number of months at the end of the reporting period. Class A indicates complete control of definite spells. References Committee on Hearing and Equilibrium guidelines for the diagnosis and evaluation of therapy in Meniere’s disease Otolaryngol Head Neck Surg 1995:113:181-5. Monsell, E. New and revised reporting guidelines from the Committee on Hearing and Equilibrium Otolaryngol Head Neck Surg 1995;113:176-8.
Communication from the Committee on Equilibrium
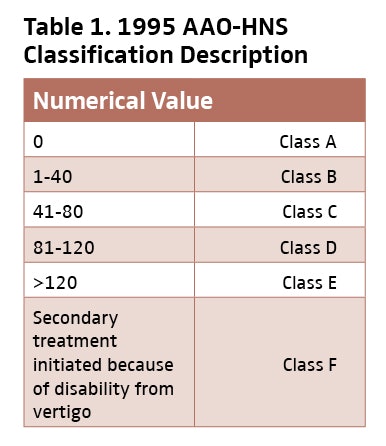
The 1995 Committee on Hearing and Equilibrium Guidelines for the Diagnosis and Evaluation of Therapy in Meniere’s Disease established a practical and useful framework for the reporting of results in Meniere’s treatment and outcomes research, by comparing the frequency of definite attacks for the period six months before treatment compared with the interval occurring between 18 and 24 months after treatment (ref1). Class A-F results were defined, based on a comparison of the frequency of spells (see Table 1). Class F outcome was reported if secondary treatment was initiated due to disability from vertigo. As Meniere’s disease has evolved from a “disease” to Meniere’s syndrome, and as treatment options have changed since the initial publication in 1995, the Committee on Equilibrium has prepared this document to serve as an assessment and publication standard for current and future reporting on Meniere’s syndrome.
With the advent of intratympanic therapy for Meniere’s syndrome, the accurate application of the prior guidelines to reports including intratympanic therapy as a treatment was impossible, since intratympanic therapy is often performed repeatedly, dependent on symptom severity. As such, the committee suggests considering intratympanic therapies as “intent to treat” events. The patient would enter the “intratympanic steroid treatment” or “intratympanic gentamicin treatment” arm, and irrespective of the number of treatments, outcome at 18 months to 24 months could be compared to other treatments, such as medical management or surgery. Progression to a secondary treatment other than the original “intent to treat” arm would still be considered a class F event. Patients in the “intratympanic steroid intent to treat” arm would be classified as class F if they entered the “intratympanic gentamicin intent to treat” arm.
The frequency of intratympanic treatment could also be reported in any publication, and would add additional relevant detail to the evaluation of this treatment.
The committee considered whether outcome reporting based totally on frequency of attacks was an optimal strategy. The current A-F reporting guidelines are based solely on frequency of attacks, are in wide use, and have been a standard of comparability in the literature. However, more information regarding the severity of attacks would be useful in evaluating therapies.
The committee recommended the following five-point scale of daily vertigo severity, with acknowledgement that other daily vertigo severity scales are also in use:
0—No vertigo.
1—Mild attack—brief episode of vertigo lasting less than 20 minutes and/or vague sense of disequilibrium lasting less than two hours.
2—Moderate attack—vertigo lasting between 20 to 60 minutes and/or disequilibrium lasting greater than two hours with reduction in daily activities from 0 percent to 50 percent.
3—Severe attack—vertigo lasting more than one hour with or without accompanying nausea and vomiting, with or without lingering disequilibrium lasting greater than two hours with reduction in daily activities. between 50 percent to 100 percent.
4—Extreme attack—vertigo lasting more than one hour with nausea and vomiting and persistent lingering severe disequilibrium requiring bed rest the entire day.
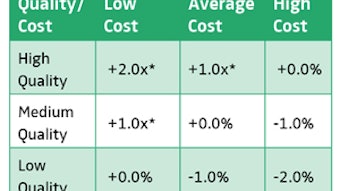
The numerical value is the ratio of the average number of vertigo spells during the pretreatment period divided by the average number of vertigo spells for the same number of months at the end of the reporting period.
Class A indicates complete control of definite spells.
References
Committee on Hearing and Equilibrium guidelines for the diagnosis and evaluation of therapy in Meniere’s disease Otolaryngol Head Neck Surg 1995:113:181-5.
Monsell, E. New and revised reporting guidelines from the Committee on Hearing and Equilibrium Otolaryngol Head Neck Surg 1995;113:176-8.