CMS Quality Reporting Initiatives Fact Sheets
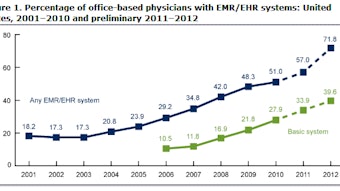
This is a pivotal year for physicians as the Centers for Medicare & Medicaid Services (CMS) now begins to apply penalties across three of its quality initiatives. In 2015, physicians will be subject to financial penalties, known as payment adjustments, for the first time for the Electronic Health Record (EHR) Meaningful Use Incentive Program and Physician Quality Reporting System (PQRS). The 2015 EHR and PQRS penalties are based on participation and reporting in 2013. Penalties also increase for failing to participate and meet the e-Prescribing (eRx) Incentive Program reporting criteria in 2013. In order to help you understand the reporting requirements for these quality initiatives, the Academy has created one-page fact sheets for each of the CMS initiatives. These fact sheets include a brief overview of the program; provide information on how you and your practice can successfully meet the reporting criteria, earn incentives, avoid payment reductions; and direct you to additional resources to help you in 2013. For information on all of these programs, visit the Academy’s CMS Quality Initiatives webpage at www.entnet.org/cmspenalties.
This is a pivotal year for physicians as the Centers for Medicare & Medicaid Services (CMS) now begins to apply penalties across three of its quality initiatives. In 2015, physicians will be subject to financial penalties, known as payment adjustments, for the first time for the Electronic Health Record (EHR) Meaningful Use Incentive Program and Physician Quality Reporting System (PQRS). The 2015 EHR and PQRS penalties are based on participation and reporting in 2013. Penalties also increase for failing to participate and meet the e-Prescribing (eRx) Incentive Program reporting criteria in 2013. In order to help you understand the reporting requirements for these quality initiatives, the Academy has created one-page fact sheets for each of the CMS initiatives. These fact sheets include a brief overview of the program; provide information on how you and your practice can successfully meet the reporting criteria, earn incentives, avoid payment reductions; and direct you to additional resources to help you in 2013. For information on all of these programs, visit the Academy’s CMS Quality Initiatives webpage at www.entnet.org/cmspenalties.