3P Update: EHR Cloning and Provider Responsibility
The Physician Payment Policy Workgroup (3P), co-chaired by James C. Denneny III, MD, and Michael Setzen, MD, is the senior advisory body to Academy leadership and staff on issues related to socioeconomic advocacy, regulatory activity, coding or reimbursement, and practice services or management. 3P wants members to take note that 2013 represents a shift in the use of Electronic Health Records (EHR) as the program administered by the Centers for Medicare & Medicaid Services (CMS) incorporate penalties for unsuccessful participants for the first time. Reporting in 2013 will be used to determine whether or not an eligible professional will be subjected to a one percent Medicare payment reduction in 2015. These penalties increase annually as the program advances. Penalties and incentives are determined on an annual basis, meaning if a physician attests or fails to successfully attest in 2013, it only applies to the incentive payment in 2014, or the penalty assessed in 2015. It is important to note that you must continue to successfully report on an annual basis to avoid penalties and earn incentive payments. How Are Your Colleagues Doing? In the last few years, the Health Policy department has seen an increase in the number of physicians and eligible professionals utilizing EHRs in their practice. According to a December 2012 Centers for Disease Control and Prevention (CDC) report, 72 percent of office-based physicians used an EHR system in 2012, up from 48 percent in 2009. Forty percent of all office-based physicians said their system met the basic Office of the National Coordinator of Health Technology (ONC) and CMS certification criteria. This is an increase of 18 percent since 2009. The same report stated that 66 percent of office-based physicians reported that they planned to apply, or already had applied, for “meaningful use” incentives. Finally, 27 percent of office-based physicians who planned to apply or already had applied for meaningful use incentives had computerized systems with capabilities to support 13 of the “Stage 1 Core Set” objectives for meaningful use. See Figure 1. The Academy supports the continued integration of EHRs into the practices of otolaryngologist-head and neck surgeons and is working to continue to provide resources to members to best allow them to use EHRs and successfully participate in the CMS Medicare and Medicaid EHR Incentive Program. As this integration continues and increases in the coming years, physicians and their staff should be aware of the responsibilities they face with the implementation or continued use of an EHR in their practice and actively protect themselves and their practices. This article, while not designed to scare you or deter you from utilizing an EHR system, hopes instead to make you aware of potential issues so you can most effectively use your EHR to improve your practice while remaining vigilant to potential issues that can arise with the incorporation of an EHR system. CMS Audits Last summer, CMS began to send out letters to physicians notifying them they were chosen to be audited for their EHR Meaningful Use Stage 1 Incentive Payment. According to Jim Tate of the website HITECHAnswers, letters from the accounting firm Figliozzi and Company, the contractor chosen to administer the EHR Audit program, asked physicians to provide “proof of possession of a certified EHR technology system…documentation that proves that 50 percent or more of patient encounters during the reporting period were entered into a Certified EHR Technology system,” and “for both the Core and Menu Set Objectives/Measures: supporting documentation used during the attestation.” According to the law firm of Ober Kaler, these audits are not specifically targeting physicians, but appear to be sweeping audits to investigate incentive payments and possibly serve as the basis for future audit programs to maintain program integrity. It is important to remember several points as you use your EHR system in your practice in case you are chosen for an audit of your EHR Incentive Program payment. Key Point # 1: Keep sufficient documentation of your patient encounters, including the supporting documentation for the criteria you choose to report as part of the attestation process and any other records that could be used to prove the encounter took place during the reporting period. An EHR “does not think” and it is important to add additional relevant information regarding the patient’s problem during the visit in order to support what is being done. It is also helpful to keep records of any conversations you have with official resources like the EHR Incentive Program Information Center concerning questions about attestation. Proper Coding and Cloning: Another important point a physician and his/her office should remember refers to the billing associated with EHR systems. Many systems provide suggested CPT and associated ICD 9 codes to assist with the billing process. However, it is important to remember that these are suggestions, not hard facts. The responsibility for proper coding rests with the physician and his office, not the EHR or the vendor that developed the system. “Upcoding” and “cloning” are two terms that have quickly become associated with issues surrounding EHR coding and present challenges to physicians when it comes to protecting themselves. Cloning refers to an EHR system automatically copying and pasting notes from a previous patient encounter into a new documentation of examination, and when coupled with new information input into the note, could lead to the EHR suggesting a higher level of E/M exam. In any case, the physician, working with his staff, is ultimately responsible for ensuring correct coding and need to code based on 1995 or 1997 E/M coding guidelines. One way to help ensure correct coding is to work with the vendor to allow the prior information to be seen, but not “counted” as part of the visit. Speak with your vendor to see if your EHR system has this capability. Key Point #2: As the physician, you must ensure that you review the information included in a note and the suggested associated E/M code and confirm the proper codes are reported. You can review your contract with your vendor, but in many cases, vendors explicitly state they are not responsible for any coding submitted by a physician and it is the responsibility of the physician to make sure they are coding correctly. Potential Liability Issues: Along with potential audits associated with the use of an EHR, physicians must also assess the potential personal and medical liability issues associated with the use of an EHR. Sensitive patient data is stored and transmitted via an EHR and it is essential you work to ensure this information is protected. Many EHRs meet the specified security criteria set by ONC, but it is important that you check with your vendor to verify your system meets the necessary security criteria and is up to date to protect against threats. According to The Doctors Company, another issue physicians must be aware of is “alert fatigue.” Many EHRs have the capability to alert the physician of different warnings including drug-drug interactions, drug allergies, or other designated alters. “Because of ‘alert fatigue,’ there is a danger that doctors may ignore, override, or disable alerts, warnings, reminders, and embedded practice guidelines. If it can be shown that following an alert or a guideline would have prevented an adverse patient event, the doctor may be found liable for failing to follow it.” Key Point #3: Work with your vendor and your attorney to understand your rights and responsibilities when it comes to potential medical and personal liability risks when using an EHR in your practice. Resources to Help: The Academy does have resources designed to help you navigate the world of Meaningful Use and the policies that govern the program, which can be found on the Academy’s EHR webpage at http://www.entnet.org/Practice/ONC.cfm. Here you can find the Academy’s comment letters and summaries, as well as details on the specific objectives and measures in meaningful use. The Academy continues to comment on current and future regulations based upon our members’ needs and experiences. If you have specific questions regarding your system or your potential liability, the Academy recommends contacting your vendor, consultant, or an attorney that can best help you with your specific and unique case. However, the Academy can direct you to several resources designed to help navigate the world of electronic health records and your practice. Government Agency Resources The Agency for Healthcare Research and Quality (AHRQ) has developed a guide to reducing unintended consequences when using an EHR. http://www.ucguide.org/index.html. The CMS EHR Incentive Program Information Center is a toll free hotline that helps answer all physician questions regarding EHRs. (888) 734-6433, TTY (888) 734-6563. CMS EHR Incentive Program criteria and information. http://cms.gov/ehrincentiveprograms. Additional Resources Karen Zupko and the AAO-HNS provide workshops that can help you learn how to code properly and help protect against audits. http://www.entnet.org/ConferencesAndEvents/codingworkshops.cfm. The Doctors Company, the largest medical malpractice insurer, has a useful page full of resources to navigate physician liability when it comes to EHRs. http://www.thedoctors.com/KnowledgeCenter/EHRandTelemedicine/index.htm. For additional questions about electronic health records or meaningful use criteria, email Joe Cody, MA, health policy analyst at healthpolicy@entnet.org.
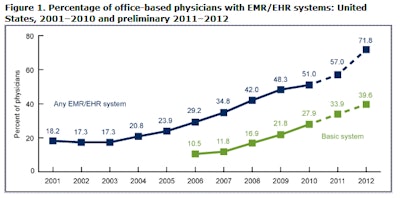 Figure 1. Physician Use of EHRs and their Capabilities. Source: http://www.cdc.gov/nchs/data/databriefs/db111.htm
Figure 1. Physician Use of EHRs and their Capabilities. Source: http://www.cdc.gov/nchs/data/databriefs/db111.htmThe Physician Payment Policy Workgroup (3P), co-chaired by James C. Denneny III, MD, and Michael Setzen, MD, is the senior advisory body to Academy leadership and staff on issues related to socioeconomic advocacy, regulatory activity, coding or reimbursement, and practice services or management. 3P wants members to take note that 2013 represents a shift in the use of Electronic Health Records (EHR) as the program administered by the Centers for Medicare & Medicaid Services (CMS) incorporate penalties for unsuccessful participants for the first time.
Reporting in 2013 will be used to determine whether or not an eligible professional will be subjected to a one percent Medicare payment reduction in 2015. These penalties increase annually as the program advances. Penalties and incentives are determined on an annual basis, meaning if a physician attests or fails to successfully attest in 2013, it only applies to the incentive payment in 2014, or the penalty assessed in 2015. It is important to note that you must continue to successfully report on an annual basis to avoid penalties and earn incentive payments.
How Are Your Colleagues Doing?
In the last few years, the Health Policy department has seen an increase in the number of physicians and eligible professionals utilizing EHRs in their practice. According to a December 2012 Centers for Disease Control and Prevention (CDC) report, 72 percent of office-based physicians used an EHR system in 2012, up from 48 percent in 2009. Forty percent of all office-based physicians said their system met the basic Office of the National Coordinator of Health Technology (ONC) and CMS certification criteria. This is an increase of 18 percent since 2009. The same report stated that 66 percent of office-based physicians reported that they planned to apply, or already had applied, for “meaningful use” incentives. Finally, 27 percent of office-based physicians who planned to apply or already had applied for meaningful use incentives had computerized systems with capabilities to support 13 of the “Stage 1 Core Set” objectives for meaningful use. See Figure 1.
The Academy supports the continued integration of EHRs into the practices of otolaryngologist-head and neck surgeons and is working to continue to provide resources to members to best allow them to use EHRs and successfully participate in the CMS Medicare and Medicaid EHR Incentive Program. As this integration continues and increases in the coming years, physicians and their staff should be aware of the responsibilities they face with the implementation or continued use of an EHR in their practice and actively protect themselves and their practices. This article, while not designed to scare you or deter you from utilizing an EHR system, hopes instead to make you aware of potential issues so you can most effectively use your EHR to improve your practice while remaining vigilant to potential issues that can arise with the incorporation of an EHR system.
CMS Audits
Last summer, CMS began to send out letters to physicians notifying them they were chosen to be audited for their EHR Meaningful Use Stage 1 Incentive Payment. According to Jim Tate of the website HITECHAnswers, letters from the accounting firm Figliozzi and Company, the contractor chosen to administer the EHR Audit program, asked physicians to provide “proof of possession of a certified EHR technology system…documentation that proves that 50 percent or more of patient encounters during the reporting period were entered into a Certified EHR Technology system,” and “for both the Core and Menu Set Objectives/Measures: supporting documentation used during the attestation.”
According to the law firm of Ober Kaler, these audits are not specifically targeting physicians, but appear to be sweeping audits to investigate incentive payments and possibly serve as the basis for future audit programs to maintain program integrity. It is important to remember several points as you use your EHR system in your practice in case you are chosen for an audit of your EHR Incentive Program payment.
Key Point # 1: Keep sufficient documentation of your patient encounters, including the supporting documentation for the criteria you choose to report as part of the attestation process and any other records that could be used to prove the encounter took place during the reporting period. An EHR “does not think” and it is important to add additional relevant information regarding the patient’s problem during the visit in order to support what is being done. It is also helpful to keep records of any conversations you have with official resources like the EHR Incentive Program Information Center concerning questions about attestation.
Proper Coding and Cloning: Another important point a physician and his/her office should remember refers to the billing associated with EHR systems. Many systems provide suggested CPT and associated ICD 9 codes to assist with the billing process. However, it is important to remember that these are suggestions, not hard facts. The responsibility for proper coding rests with the physician and his office, not the EHR or the vendor that developed the system. “Upcoding” and “cloning” are two terms that have quickly become associated with issues surrounding EHR coding and present challenges to physicians when it comes to protecting themselves.
Cloning refers to an EHR system automatically copying and pasting notes from a previous patient encounter into a new documentation of examination, and when coupled with new information input into the note, could lead to the EHR suggesting a higher level of E/M exam. In any case, the physician, working with his staff, is ultimately responsible for ensuring correct coding and need to code based on 1995 or 1997 E/M coding guidelines. One way to help ensure correct coding is to work with the vendor to allow the prior information to be seen, but not “counted” as part of the visit. Speak with your vendor to see if your EHR system has this capability.
Key Point #2: As the physician, you must ensure that you review the information included in a note and the suggested associated E/M code and confirm the proper codes are reported.
You can review your contract with your vendor, but in many cases, vendors explicitly state they are not responsible for any coding submitted by a physician and it is the responsibility of the physician to make sure they are coding correctly.
Potential Liability Issues: Along with potential audits associated with the use of an EHR, physicians must also assess the potential personal and medical liability issues associated with the use of an EHR. Sensitive patient data is stored and transmitted via an EHR and it is essential you work to ensure this information is protected. Many EHRs meet the specified security criteria set by ONC, but it is important that you check with your vendor to verify your system meets the necessary security criteria and is up to date to protect against threats.
According to The Doctors Company, another issue physicians must be aware of is “alert fatigue.” Many EHRs have the capability to alert the physician of different warnings including drug-drug interactions, drug allergies, or other designated alters. “Because of ‘alert fatigue,’ there is a danger that doctors may ignore, override, or disable alerts, warnings, reminders, and embedded practice guidelines. If it can be shown that following an alert or a guideline would have prevented an adverse patient event, the doctor may be found liable for failing to follow it.”
Key Point #3: Work with your vendor and your attorney to understand your rights and responsibilities when it comes to potential medical and personal liability risks when using an EHR in your practice.
Resources to Help: The Academy does have resources designed to help you navigate the world of Meaningful Use and the policies that govern the program, which can be found on the Academy’s EHR webpage at http://www.entnet.org/Practice/ONC.cfm. Here you can find the Academy’s comment letters and summaries, as well as details on the specific objectives and measures in meaningful use. The Academy continues to comment on current and future regulations based upon our members’ needs and experiences.
If you have specific questions regarding your system or your potential liability, the Academy recommends contacting your vendor, consultant, or an attorney that can best help you with your specific and unique case. However, the Academy can direct you to several resources designed to help navigate the world of electronic health records and your practice.
Government Agency Resources
- The Agency for Healthcare Research and Quality (AHRQ) has developed a guide to reducing unintended consequences when using an EHR. http://www.ucguide.org/index.html.
- The CMS EHR Incentive Program Information Center is a toll free hotline that helps answer all physician questions regarding EHRs. (888) 734-6433, TTY (888) 734-6563.
- CMS EHR Incentive Program criteria and information. http://cms.gov/ehrincentiveprograms.
Additional Resources
- Karen Zupko and the AAO-HNS provide workshops that can help you learn how to code properly and help protect against audits. http://www.entnet.org/ConferencesAndEvents/codingworkshops.cfm.
- The Doctors Company, the largest medical malpractice insurer, has a useful page full of resources to navigate physician liability when it comes to EHRs. http://www.thedoctors.com/KnowledgeCenter/EHRandTelemedicine/index.htm.
For additional questions about electronic health records or meaningful use criteria, email Joe Cody, MA, health policy analyst at healthpolicy@entnet.org.