World Sinus Health Awareness Month: Growing Concern Regarding Air Pollution
A review of the evidence on the impact of air pollution on sinonasal inflammatory diseases, specifically allergic rhinitis and chronic rhinosinusitis and implications for clinical practice.
Victoria S. Lee, MD, Li-Xing Man, MD, MSc, MPA, Edward D. McCoul, MD, MPH, and Patricia L. Purcell, MD, MPH, on behalf of the Outcomes Research and Evidence-Based Medicine Committee

This Bulletin article reviews the evidence on the impact of air pollution on sinonasal inflammatory diseases, specifically allergic rhinitis (AR) and chronic rhinosinusitis (CRS), and discusses implications for clinical practice.
What Is the Evidence on the Association of Air Pollution and AR and CRS?
Published in 2018, the initial International Consensus Statement on Allergic Rhinitis (ICAR:AR) suggested there is “minimal or no significant associations between air pollutants and AR development.”3 Indicative of the rapid advancement of evidence to support an association, however, the updated 2023 ICAR:AR noted that the evidence demonstrating the detrimental role of air pollution on AR prevalence and severity had “certainly advanced.”4 For example, exposure to high levels of traffic pollution-related NO2 and exhaust particles during the first year of life has been associated with increased risk of sensitization to aeroallergens in early childhood.5,6,7
A variety of pathophysiologic mechanisms has been proposed:
- oxidative stress leading to epigenetic modifications, tissue inflammation, and apoptosis,
- enhancement of allergic airway hypersensitivity, evidenced by increased type 2 inflammatory marker expression,
- increased amount and potency of allergens via triggering of allergen release, enhancement of antigenic properties of allergens, increased penetration of allergens due to compromised airway protective factors, and binding of free allergens and pollutants that enable travel and can cross-link receptors to trigger exaggerated responses,
- and neurogenic-mediated pathways.8,9,10
An additional question is whether air pollution exposure in utero has an impact on AR or CRS development in children. A 2023 systematic review summarized the existing literature, identifying eight studies looking at variety of traffic-related air pollutants.11 In the studies on traffic-related air pollutant exposure during pregnancy, exposure was positively associated with the development of AR in children. Suggested mechanisms include placental transmission and destabilization of the epithelial barrier of the sinuses and nose.
A 2022 systematic review synthesized the available evidence to date on the association of pollution and CRS, identifying ten studies.12 Four studies conducted in different geographical regions examined CRS incidence and prevalence; three studies showed an association with air pollution and one study showed an association between CRS prevalence but not incidence and air pollution. Four studies, three by the same author group, evaluated CRS disease severity and quality of life; in two out of the four studies, some of the disease severity metrics were worse with higher pollutant (particulate matter and black carbon) levels in CRS without polyps but not CRS with polyps. Two studies assessed CRS histopathology and microbiology; reported findings with pollutant exposure included inflammatory changes, presence of Charcot-Leyden crystals, eosinophilic aggregation, presence of eosinophilic markers, and lower levels of Corynebacterium. In sum, there is mixed evidence to support an association between pollution and CRS with high data heterogeneity in pollutant types and outcome measures assessed. Of note, the data since the publication of this review has grown rapidly, further supporting an association.13,14,15,16
From an epidemiologic standpoint, future studies are needed with larger sample sizes, more homogeneous outcome measures, and healthy control comparison populations. Many studies have used home addresses to determine pollutant exposure, which is imprecise. Future studies should incorporate more precise methodologies for determining pollutant exposure.11,12 Research is also needed to better understand the cellular mechanisms underlying the epidemiologic associations observed. As part of this, there is also a need to identify biomarkers of pollution exposure, which not only has a research benefit but also potential diagnostic, prognostic, and therapeutic benefits.17
Practical Tips for Clinicians
Environmental exposures and air quality are increasingly recognized as playing a role in development of AR and CRS; therefore, it is important to take a thorough environmental history. Important aspects of indoor environments (home, school, and work) include building history and physical appearance, heating and cooling systems, windows and coverings, water and moisture, flooring, pillows and bedding, pests, pets, air quality, chemical and cleaning agent use, and substance use. Key aspects of the outdoor environment around home, school, and work include the proximity of high traffic, construction work, garbage dumps, water, weeds and farm fields with burnings and other smoke and fire hazards, and industries and mills. With a thorough environmental history, clinicians may better identify major environmental triggers for a patient’s sinonasal symptoms and better counsel patients on avoidance and mitigation strategies.
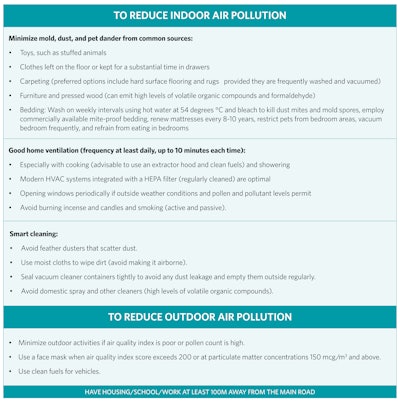
Non-pharmacologic measures to reduce indoor and outdoor air pollution are listed in Table 1.8,18 Currently, there is little to no evidence on pharmacologic therapy for patients exposed to specific pollutants, and more research is needed in this area.
Table 1: Non-pharmacological measures to reduce air pollution
Conclusions
Increasing evidence supports an association between air pollution, a leading cause of death globally that exacerbates health disparities, and AR and CRS. Thus, a detailed environmental history is important in assessing patients with sinonasal symptomatology. Based on this history, there are non-pharmacologic measures that we can recommend to patients to minimize the impact of air pollution and environmental factors on sinonasal symptomatology. We should act to mitigate detrimental air quality, which can have a negative impact on the sinuses and nose.9
References
- World Health Assembly, 68. Health and the environment: Addressing the health impact of air pollution. 2015.
- Fuller R, Landrigan PJ, Balakrishnan K, et al. Pollution and health: a progress update. Lancet Planet Health. 2022 Jun;6(6):e535-e547.
- Wise SK, Lin SY, Toskala E, et al. International Consensus Statement on Allergy and Rhinology: Allergic Rhinitis. Int Forum Allergy Rhinol. 2018 Feb;8(2);108-352.
- Wise SK, Damask C, Roland LT, et al. International consensus statement on allergy and rhinology: Allergic rhinitis - 2023. Int Forum Allergy Rhinol. 2023 Apr;13(4):293-859.
- Gruzieva O, Bellander T, Eneroth K, et al. Traffic-related air pollution and development of allergic sensitization in children during the first 8 years of life. J Allergy Clin Immunol 2012 Jan;129(1):240-246.
- Codispoti CD, LeMasters GK, Levin L, et al. Traffic pollution is associated with early childhood aeroallergen sensitization. Ann Allergy Asthma Immunol 2015 Feb;114(2):126-133.
- Sibhi H, Allen RW, Becker A, et al. Perinatal exposure to traffic-related air pollution and atopy at 1 year of age in a multicenter Canadian birth cohort study. Environ Health Perspect 2015;123:902-908.
- Naclerio R, Ansotegui IJ, Bousquet J, et al. International expert consensus on the management of allergic rhinitis (AR) aggravated by air pollutants: Impact of air pollution on patients with AR: Current knowledge and future strategies. World Allergy Organ J. 2020 Apr 3;13(3):100106.
- Pacheco SE, Guidos-Fogelbach G, Annesi-Maesano I, et al. Climate change and global issues in allergy and immunology. J Allergy Clin Immunol. 2021 Dec;148(6):1366-1377.
- Irizar H, Chun Y, Hsu H-HL, et al. Multi-omic integration reveals alterations in biology that mediate air pollutant effects on allergic rhinitis. Allergy 2024 May 26.
- Liu L, Ma J, Peng S, Xie L. Prenatal and early-life exposure to traffic-related air pollution and allergic rhinitis in children: A systematic literature review. PLoS One. 2023 Apr 20;18(4):e0284625.
- Leland EM, Vohra V, Seal SM, Zhang Z, Ramanathan M Jr. Environmental air pollution and chronic rhinosinusitis: A systematic review. Laryngoscope Investig Otolaryngol. 2022 Mar 11;7(2):349-360.
- Chen SW, Lin HJ, Tsai SC, Lin CL, Hsu CY, Hsieh TL, Chen CM, Chang KH. Exposure to Air Pollutants Increases the Risk of Chronic Rhinosinusitis in Taiwan Residents. Toxics. 2022 Apr 1;10(4):173.
- Peeters S, Wang C, Bijnens EM, Bullens DMA, Fokkens WJ, Bachert C, Hellings PW, Nawrot TS, Seys SF. Association between outdoor air pollution and chronic rhinosinusitis patient reported outcomes. Environ Health. 2022 Dec 21;21(1):134.
- Wolf JS, Papadimitriou JC, Morales RE, Califano JA 3rd, Kline NL, Bhatnagar K, Hebert AM, Taylor RJ. The association of active and passive tobacco smoke exposure with chronic rhinosinusitis symptom severity: A cross-sectional study. Int Forum Allergy Rhinol. 2022 Mar;12(3):278-285.
- Yang X, Shen S, Deng Y, Wang C, Zhang L. Air Pollution Exposure Affects Severity and Cellular Endotype of Chronic Rhinosinusitis With Nasal Polyps. Laryngoscope. 2022 Nov;132(11):2103-2110.
- Marques-da-Silva D, Videira PA, Lagoa R. Registered human trials addressing environmental and occupational toxicant exposures: Scoping review of immunological markers and protective strategies. Environ Toxicol Pharmacol. 2022 Jul;93:103886.
- Reddy KRBK, Gupta N, Bhattacharya BG, et al. Impact of Air Pollution on Allergic Rhinitis and Asthma: Consensus Statement by Indian Academy of Pediatrics. Indian Pediatr. 2021 Aug 15;58(8):765-770.