Comment in Reference to “Pediatric Rhinitis and Chronic Rhinosinusitis”
We advocate for a more comprehensive approach to the diagnosis and management of allergic rhinitis and chronic rhinosinusitis in children.
Glenis K. Scadding, MD, MA, Lars-Olaf Cardell, MD, PhD, Diego M. Conti, MD, Peter W. Hellings, MD, PhD, and Michael Blaiss, MD, on behalf of the European Forum for Research and Education in Allergy and Airway Diseases (EUFOREA)
Author disclosures appear at the end of this article.

Rhinosinusitis is common in childhood, largely relating to recurrent colds, of which the average child has six to eight per year. The priority is to decide whether the child and family have need for anything more than reassurance that aging will bring improvement, advice about not smoking, and possible use of nasal saline. This decision can be achieved by taking a general history regarding sleep, breathing, hearing, school attendance and progress, energy, exercise, and diet and by checking height, weight and looking for any co-morbidities such as asthma and otitis media with effusion (OME).1-3 A child who is failing in any of these aspects or has continuous, unabating symptoms needs further attention.4
AR is also common, often missed, and frequently mistreated. This is a pity because it can be an interruptible route to more complex airway disease such as asthma.5,6 Symptoms such as itching and eye irritation on exposure to known allergens suggest AR and should provoke IgE testing. Both AR or CRS and asthma are part of a pathophysiological continuum, which means that a patient who is not accurately diagnosed and treated may develop associated comorbidities.5,6 Timely intervention with early diagnosis and appropriate treatment, such as allergen- specific immunotherapy, is key to interrupting the process.1-5
The concept of unilaterality has been missed in the original article. Any manifestation with a unilateral presentation should make us consider situations ranging from foreign body at one end to neoplastic pathology at the other.1-3
Unremitting symptoms need proper investigation before treatment is considered. Immune deficiency, especially innate problems such as ciliary dyskinesia or cystic fibrosis, often present with airway disease. Measuring nasal nitric oxide is a quick way to check these possibilities, as is the presence of nasal polyps. Blood tests for immune deficiency should also be considered.4 The use of computed tomography (CT) scans in childhood is restricted by radiation exposure considerations7 and complicated by the fact that 46% of unselected children have abnormal sinus CTs.8 So, these should only be undertaken when deemed absolutely necessary and are not diagnostic on their own.1-3
Although we agree with the range of therapeutic options presented by Dr. Stapleton, we believe that a more holistic approach is essential, where each option is considered as a step on a pathway, only progressing in complexity where required.9 The European Forum for Research and Education in Allergy and Airway Diseases (EUFOREA) has summarised and simplified current knowledge in its “Pocket Guide to AR in Children”.1-3 The guide highlights an algorithm (Figure 1) for disease management, which sets out the actions to be taken by all levels of the healthcare system at different stages of the disease and reviews the patient's current status before offering a therapeutic alternative. This group believes that this approach is best suited to the individuality of each patient.1-3 A similar initiative is underway in paediatric CRS.
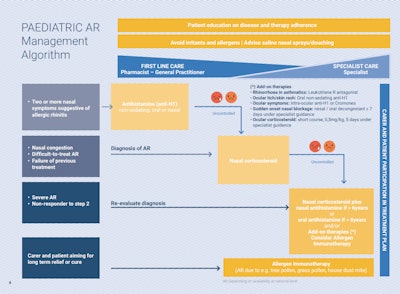 Figure 1. Pediatric AR management algorithm from the EUFOREA Pocket Guide to AR in Children.
Figure 1. Pediatric AR management algorithm from the EUFOREA Pocket Guide to AR in Children.
Surgery is not a definitive treatment in most CRS patients.10,11 Surgery prepares the groundwork so that the treatment to be applied has adequate access.12,13 Due to the inflammatory nature of CRS, surgery alone cannot be expected to interrupt the process.1-3 The possible exception to this is adenoidectomy where the adenoid is the focus of inflammation and obstruction.14
The consideration of biologics in pediatric CRS and AR is not feasible at this time in the United States because none of the relevant medications have approval in the US for such indications. Currently, for CRSwNP in the US, the lower age limit is 18 years and 6 years for asthma.15 Our group believes that the basic diagnosis must be established before moving on to more complex therapies.1-3 Multidisciplinary teams are ideal in managing difficult paediatric respiratory conditions: synergies between allergists, pediatricians, ENT specialists, and pulmonologists enhance outcomes particularly in complex cases with comorbidities like asthma.5
In summary, it is essential to consider the child as a whole to establish a diagnosis and treat both underlying pathology and co-morbidities, while explaining the situation clearly to parents and caregivers.5 The approach must only progress in complexity once a diagnosis is confirmed and it is possible to make rational use of available resources.
Author disclosures:
Glenis K. Scadding, MD: Honoraria for articles, speaker, and advisory boards: ALK, Bayer, Chiesi, GlaxoSmithKline, Haleon, Noucor, Sanofi-Regeneron, and Viatris. Chair of BSACI rhinitis guidelines; Scientific Chief Editor, Rhinology Section, Frontiers in Allergy; Vice President and AR lead for EUFOREA; Chair/member of Data Monitoring Committees on SLIT for ALK. Lars-Olaf Cardell, MD: Has received institutional grants and/or personal fees from Orion Pharma, Sanofi, GlaxoSmithKline, and ALK-Abelló. Diego M. Conti, MD: Serves as Academic Manager at EUFOREA and as an Associate Editor for Frontiers in Allergy. Peter W. Hellings, MD: Recipient of consultancy/lecture fees or unrestricted research grants from Sanofi/Regeneron, Novartis, GSK, Medtronic, and Viatris. Michael Blaiss, MD: Has been an investigator, consultant, and advisor for ALK, Amgen, and AstraZeneca.
References
- Scadding GK, Smith PK, Blaiss M, et al. Allergic rhinitis in childhood and the new EUFOREA algorithm. Front Allergy. 2021;2:706589. https://doi.org/10.3389/falgy.2021.706589.
- Hellings PW, Scadding G, Bachert C, et al. EUFOREA treatment algorithm for allergic rhinitis. Rhinology. 2020;58(6):618-622. https://doi.org/10.4193/Rhin20.246.
- Hellings PW, Fokkens WJ, Orlandi R, et al. The EUFOREA pocket guide for chronic rhinosinusitis. Rhinology. 2023 Feb 1;61(1):85-89. doi: 10.4193/Rhin22.344.
- Glenis K. Scadding, The catarrhal child, Paediatrics and Child Health, Volume 26, Issue 1, 2016, Pages 21-25, ISSN 1751-7222. https://doi.org/10.1016/j.paed.2015.08.002.
- Scadding GK, McDonald M, Backer V, et al. Pre-asthma: a useful concept for prevention and disease-modification? A EUFOREA paper. Part 1—allergic asthma. Front. Allergy 4:1291185. doi: 10.3389/falgy.2023.1291185
- Diamant Z, Jesenak M, Hanania NA, et al. EUFOREA pocket guide on the diagnosis and management of asthma: An educational and practical tool for general practitioners, non-respiratory physicians, paramedics and patients. Respir Med. 2023 Jul 28:107361. doi: 10.1016/j.rmed.2023.107361.
- https://www.cancer.gov/about-cancer/causesprevention/risk/radiation/pediatric-ct-scans
- Cotter CS, Stringer S, Rust KR, Mancuso A. The role of computed tomography scans in evaluating sinus disease in pediatric patients. Int J Pediatr Otorhinolaryngol. 1999 Oct 15;50(1):63-8. doi: 10.1016/s0165-5876(99)00204-9.
- Theeling T, Djouder C, Laurens H, Preyra JH, Shire CME, Van Staeyen E, Conti DM, Scadding GK and Hellings PW (2024) Nasal polyp syndrome: a patient-centred term for CRSwNP by EUFOREA. Front. Allergy 5:1372919. doi: 10.3389/falgy.2024.1372919.
- Fokkens WJ, Pugin B, Bachert C, et al. Rhinology Future Debates 2017 by EUFOREA: Novel treatments and surgical solutions in rhinology. Clin Otolaryngol. 2018 Dec;43(6):1429-1438. doi: 10.1111/coa.13184.
- Scadding G, Bousquet J, Bachert C, et al. Rhinology future trends: 2017 EUFOREA debate on allergic rhinitis. Rhinology. 2019 Feb 1;57(1):49-56. doi: 10.4193/Rhin18.076.
- Hellings PW, Akdis CA, Bachert C, et al. EUFOREA Rhinology Research Forum 2016: report of the brainstorming sessions on needs and priorities in rhinitis and rhinosinusitis. Rhinology. 2017 Sep 1;55(3):202-210. doi: 10.4193/Rhin17.028.
- Hellings PW. From prevention to optimal treatment in chronic rhinosinusitis. Rhinology. 2018 Dec 1;56(4):305-306. doi: 10.4193/Rhin.18.404.
- Fokkens WJ, Lund VJ, Hopkins C, Hellings PW, et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2020. Rhinology. 2020 Feb 20;58(Suppl S29):1-464. doi: 10.4193/Rhin20.600.
- Bacharier LB, Jackson DJ. Biologics in the treatment of asthma in children and adolescents. J Allergy Clin Immunol. 2023 Mar;151(3):581-589. doi: 10.1016/j.jaci.2023.01.002.