The Perfect Storm
The way forward is for us, as individuals and institutional stakeholders, to come together and respond to our legislators, regulators, and government.
 Kathleen L. Yaremchuk, MD, MSA
Kathleen L. Yaremchuk, MD, MSA
AAO-HNS/F PresidentI recently visited the Pacific Northwest and enjoyed hiking and kayaking on a chain of lakes. The trout were running, and it was an amazing pattern of individual fish, swimming in the same direction and in alignment. This pattern of swimming, I have learned, is a survival tactic and is termed in philosophy as “emergence.” It occurs when fish, geese, or groups of people demonstrate properties or behaviors that emerge only when the parts interact as a wider whole. When there are large numbers together, it is much harder for a predator to find its prey while the lone fish is easier to pick off and take advantage of.
 In the school of fish, everyone is the leader and no one is the leader. There is deliberate coordination to stay close, but not too close to impede forward progress. As the school continues its journey, a set of rules evolves that focuses on avoiding predation. If you are a fan of TED Talks, Nathan S. Jacobs does a much better job explaining this in his presentation, “How Do Schools of Fish Swim in Harmony?”
In the school of fish, everyone is the leader and no one is the leader. There is deliberate coordination to stay close, but not too close to impede forward progress. As the school continues its journey, a set of rules evolves that focuses on avoiding predation. If you are a fan of TED Talks, Nathan S. Jacobs does a much better job explaining this in his presentation, “How Do Schools of Fish Swim in Harmony?”
Schools of fish, geese migrating, the sand on the beach, or snowflakes during a storm individually do not have the impact that is seen when they gather together. The takeaway is it isn’t necessary for someone to be in charge if there are rules and conditions in place so that habits develop that turn chaos into order. Last month, we discussed how we as academics, private practice, and employed otolaryngologists are stronger together. The theory of emergence explains how we can move forward with strength without impeding one another.
All of that led me to think about the 8.42% Medicare cuts that are scheduled to occur January 1, 2023. How did we get to this significant cut again? It may be described as the result of a perfect storm or an example of kicking the can down the road. This time, there are two different hits that are coming our way:
1. Medicare PAYGO
- The American Rescue Plan Act (ARP) of 2021 increased spending without offsets to other federal programs. Under statutory Pay-As-You-Go (PAYGO) rules, increases to the federal deficit automatically trigger an additional series of across-the-board reductions to federal programs. According to the Congressional Budget Office, the ARP created a 4.0% cut or $36 billion for Medicare providers per year, which would have a substantial impact on the delivery of care to our patient community.
2. Changes to the Medicare Conversion Factor
- Last year, Congress passed a temporary 3% patch to the Medicare conversion factor, which converts the relative value units into an actual dollar amount. Medicare updates the conversion factor on an annual basis according to a formula specified by statute, within the constraints of Medicare’s budget-neutral financing system. Although the patch allowed for a temporary stabilization in provider reimbursement, proposed changes to the Physician Fee Schedule for 2023 will once again cut reimbursement to providers during a critical time. Next year’s proposed Medicare Physician Fee Schedule would decrease the conversion factor by 4.42%.
The above-mentioned 8.42% pending cuts set to take place January 1, 2023, are on top of the additional 2% Medicare sequester cuts that already took effect on July 1, 2022.
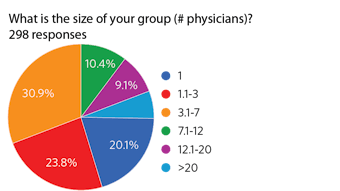
To try and tie everything together, the idea that any one otolaryngologist can impact Medicare reimbursement on their own is futile. However, the Academy’s 8,800 U.S.-based otolaryngologists who are impacted by this can “swim” in a way that can impact the reimbursement war and prove once again, we are stronger together.
As providers, we are being seen as prey by insurance companies and the government. We are needed to provide access and yet are being expected to provide services for less remuneration while we experience increasing inflation, supply chain delays, and staffing shortages.
The way forward is for us, as individuals and institutional stakeholders, to come together and respond to our legislators, regulators, and government. Our practices and healthcare institutions are currently experiencing losses and the pending 8.42% decrease by our single largest payer is not sustainable for 2023. No matter how we see ourselves, we have a much better chance of not being picked off individually if we support each other in advocacy by the Academy and other medical societies to prevent the planned Medicare reimbursement decreases for physicians.