Private Practice Study Group Survey: Emergency Room Coverage in Private Practice
The Business of Medicine in 2022 is challenging. Decreasing reimbursement, increasing workloads, and skyrocketing overhead means that every workday minute spent not providing reimbursed patient care negatively impacts a practice’s financial viability.
Marc G. Dubin, MD (PPSG Chair), David E. Melon, MD (PPSG Vice Chair), and Daniel R. Gold, MD, Annette M. Pham, MD, and Melanie Wilson Seybt, MD (PPSG Executive Committee Members)
The Business of Medicine in 2022 is challenging. Decreasing reimbursement, increasing workloads, and skyrocketing overhead means that every workday minute spent not providing reimbursed patient care negatively impacts a practice’s financial viability. One of these challenges for physicians and independent practices is health systems’ mandate for the provision of emergency coverage. Time out of the office as well as the mental and physical toll of this uncompensated coverage has led some to question, “Is this too much in the current environment?” The Academy’s updated Position Statement: Reimbursement for Taking Hospital Call suggests the answer is, “Yes.”
The Position Statement highlights that: “Otolaryngologists have graciously accepted this responsibility in the past as a requirement related to their utilization of hospital services. Many otolaryngologists no longer have the former tight hospital links, in addition to lacking contractual relationships with the hospital’s payers, and this effectively results in the physician providing uncompensated or undercompensated care. Additionally, such in-hospital care often delays care to the ill patients waiting in their office and can adversely affect the physician’s quality of life. Given the evolving reimbursement models and increasing overhead expenses, including the additional liability associated with providing emergency care, these costs to physicians can no longer be sustained. Most otolaryngologists still practice as a small business, a small group, or a solo practice. Accordingly, providing uncompensated hospital services adversely impacts their business and compromises their ability to provide quality care to their patients.” (Source: https://www.entnet.org/resource/position-statement-reimbursement-for-taking-hospital-call/)
Compensation for Call Coverage: Have Efforts Been Successful?
In 2017, the AAO-HNS Board of Governors (BOG) surveyed their constituent societies’ membership and received 677 responses. Among the heterogenous practice settings of academics, hospital-employed, military, and self-employed independent physicians, a reported 50% were financially compensated for on-call coverage. Additionally, 90% were mandated to provide unassigned emergency call either by hospital bylaws, departmental requirements, or employer mandates. (Source: https://bulletin.entnet.org/home/article/21246964/board-of-governors-socioeconomic-grassroots-committee-emergency-room-call-survey-results)
Recently, the Private Practice Study Group (PPSG) surveyed its membership (n=566) on the matter. Members expressed unique challenges to providing efficient emergency care: lack of support/infrastructure, physical distance from the health centers, lack of electronic health record interoperability, and financial loss for uncompensated emergency care among others. Given these unique demands that uncompensated emergency call coverage places on private practitioners, the goal was to assess the evolving emergency room coverage trends.
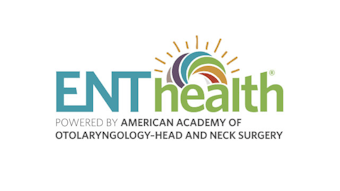
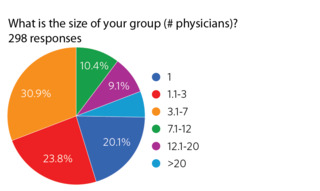 Figure 1. Size of physician group.298 PPSG members responded with a response rate of 52.7%. Among respondents, 93.6% were a partner/owner or employed in a physician-owned independent practice. The remainder were employed by or contracted by a healthcare system. 48.7% were less than 50 years old, 20.7% were between 50-65 years old, and 7.4%
Figure 1. Size of physician group.298 PPSG members responded with a response rate of 52.7%. Among respondents, 93.6% were a partner/owner or employed in a physician-owned independent practice. The remainder were employed by or contracted by a healthcare system. 48.7% were less than 50 years old, 20.7% were between 50-65 years old, and 7.4% 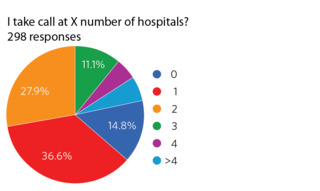 Figure 2. Number of hospitals covered on call.were over age 65. Interestingly, 20.1% of respondents were in solo practice while 74.8% of respondents were in groups of seven physicians or smaller (Figure 1). 74.5% were not fellowship trained and 66.2% were at institutions that have a trauma center (any trauma level designation).
Figure 2. Number of hospitals covered on call.were over age 65. Interestingly, 20.1% of respondents were in solo practice while 74.8% of respondents were in groups of seven physicians or smaller (Figure 1). 74.5% were not fellowship trained and 66.2% were at institutions that have a trauma center (any trauma level designation).
Most respondents (64.5%) take call at one or two hospitals, while 9.7% take call at four or more (Figure 2).
 Figure 3. Number of ENT physicians in call rotation.Regarding the frequency of call, 32.2% had four or fewer ENTs in the ER rotation, while 3.4% responded that they were the only ENT on-call for their center. The most frequent response was five to seven physicians in the call rotation with 29.2% (Figure 3).
Figure 3. Number of ENT physicians in call rotation.Regarding the frequency of call, 32.2% had four or fewer ENTs in the ER rotation, while 3.4% responded that they were the only ENT on-call for their center. The most frequent response was five to seven physicians in the call rotation with 29.2% (Figure 3).
Of this population of private practitioners, 83.3% took emergency call coverage, with 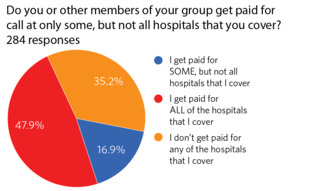 Figure 4. Percentage of paid emergency call.74.8% of the respondents being required by their hospital to do so. Of those that take emergency call, 66.8% do get paid. However, only 47.9% of respondents are compensated at all the hospitals they cover (Figure 4). Interestingly, of those that knew the answer (n=226), 23% responded that although they do not get paid for call at their hospital, they know that other service lines at their hospital are paid for call.
Figure 4. Percentage of paid emergency call.74.8% of the respondents being required by their hospital to do so. Of those that take emergency call, 66.8% do get paid. However, only 47.9% of respondents are compensated at all the hospitals they cover (Figure 4). Interestingly, of those that knew the answer (n=226), 23% responded that although they do not get paid for call at their hospital, they know that other service lines at their hospital are paid for call.
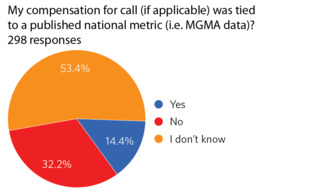 Figure 5. Call compensation based on national metric.Although the survey intentionally did not seek to measure specific compensation amounts for on-call coverage, 64.8% who are compensated were able to negotiate their call remuneration with the hospital. Only 14.4% reported a negotiated compensation based on a national metric (i.e., MGMA data), while the majority (53.4%) did not know what the compensation was based upon (Figure 5). Furthermore, 56.5% of those who were paid for ER calls felt they are not compensated adequately for their services, and only 25.9% confirmed that they were being compensated for the uninsured patients whom they provide care for while on ER call.
Figure 5. Call compensation based on national metric.Although the survey intentionally did not seek to measure specific compensation amounts for on-call coverage, 64.8% who are compensated were able to negotiate their call remuneration with the hospital. Only 14.4% reported a negotiated compensation based on a national metric (i.e., MGMA data), while the majority (53.4%) did not know what the compensation was based upon (Figure 5). Furthermore, 56.5% of those who were paid for ER calls felt they are not compensated adequately for their services, and only 25.9% confirmed that they were being compensated for the uninsured patients whom they provide care for while on ER call.
Regarding assistance when on call, only 21.1% had an advanced practice provider (APP) who helped “all the time” (12.4%) or “sometimes” (8.7%), while only 8.7% had a resident who assisted “all” or “some of the time.” Of those that used an app, 90.3% paid for this coverage assistance themselves or within their call group. Additionally, consistent with the previous BOG survey data from 2017, 47.9% felt that they were at least sometimes asked to consult, render an opinion on, or direct care outside the scope of practice of an otolaryngologist.
When taken as a whole, these data present an interesting picture of ER call coverage in the otolaryngology private practice community in the United States. Although a majority of the respondents are being compensated, most do not feel that this compensation is adequate, and a majority are being compensated based on unknown metrics.
It is hoped that knowing that the supermajority of private practice otolaryngologists are now being compensated—albeit at what many feel is a below-market rate—we will be empowered to advocate for ourselves and negotiate from a position of strength that supports compensation for call at fair market value.