Models of Otolaryngology Practice: Employment Dilemmas Stocked by COVID-19
The COVID-19 pandemic has afflicted every person, every family, every medical practice, the entire healthcare industry, and the overall economic fabric of this nation and abroad.
Ken Yanagisawa, MD, AAO-HNS/F President-Elect; and James C. Denneny III, MD, AAO-HNS/F Executive Vice President and CEO
 Ken Yanagisawa, MD
Ken Yanagisawa, MD
AAO-HNS/F President-Elect James C. Denneny III, MD
James C. Denneny III, MD
AAO-HNS/F Executive Vice President and CEO
The COVID-19 pandemic has afflicted every person, every family, every medical practice, the entire healthcare industry, and the overall economic fabric of this nation and abroad. With shutdowns initially taking place in the spring of 2020, practices suffered enormous physical, emotional, and economic challenges necessitating a complete reconfiguration and overhaul of the normal workflows in our offices, hospitals, and surgery centers, including patient prescreens, office space modifications, protections for our staff, patients, and providers, and continuous cleaning and disinfecting of our office spaces, not to mention the personal health risks presented to ourselves and our staffs.
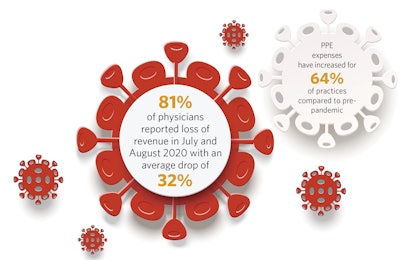
According to a recent American Medical Association (AMA) survey1, 81% of physicians reported loss of revenue in July and August 2020 with an average drop of 32%. Patient volumes are dramatically decreased in many areas and capacities are limited due to the myriad safety measures required. Personal Protective Equipment (PPE) expenses have increased for 64% of practices compared to pre-pandemic, and the limited availability has led, at times, to price gouging behaviors that health centers and practices have had to endure and overcome.
Yet, we have managed to survive this onslaught, and as we have all learned how to practice as safely as possible in this new environment, practices are gradually rebuilding and rebounding, and patients are increasingly seeking in-person medical care.
Also significantly affected by all this turmoil have been our graduating otolaryngology residents and fellows who seek to identify opportunities that best fit their desired employment situations in academic and private-practice settings. Most traditional employment techniques and planning have been disrupted by COVID-19, and our graduates and members are facing a new set of challenges in procuring jobs as attending physicians. Frequent travel restrictions, as well as the unprecedented transformation of our AAO-HNSF 2020 Annual Meeting & OTO Experience from a live event to a virtual one, have prevented in-person interviews and meetings. Virtual conversations serve a valuable purpose but cannot replace live face-to-face meetings where physical workspaces can be toured; where the flow and interaction of staff, patients, and providers can be experienced; and for the crucial nonverbal cues that video conferencing cannot convey. The current situation prevents candidates from evaluating the full experience of employment locations that they are not already familiar with. Where they and their families will live remains a critical determinant in employment selection.
The dreams and aspirations of many 2020 and 2021 graduates have been adversely impacted by challenging obstacles in procuring attending jobs. Concerns for their future have also impacted their wellness. Offers that had been made were rescinded, positions were unilaterally changed from full-time to part-time, and employment deferrals for six or more months were enforced—all due to the markedly diminished patient flow and resultant financial impacts ushered in so rapidly and unexpectedly by COVID-19. In some cases, the positions that were deferred have already been filled by the corps of deferred applicants, reducing the available openings for our current graduates.
Sadly, some practices were forced to close due to the pandemic. Others had to partner with larger systems to remain financially viable. Most practices that remained solvent had to reduce or temporarily close office hours, rapidly incorporate telehealth options, and were forced into the unanticipated and unimaginable need to layoff and furlough loyal office staff. The economic impacts even led to reduced hours and terminations of recently hired physicians in addition to deferred compensation for partner physicians.
Several strategies have proven valuable to mitigate these COVID-19-induced employment dilemmas for our graduates and members.
First, keep an open mind as you explore future practice opportunities. Flexibility can open doors. Rigidity will limit options. Be willing to think outside of the pre-2020 box. Opportunities do exist in both academic and private practice settings. Location and lifestyle considerations were among the most important factors prior to 2020 and remain important, but currently, availability and practice settings with economic stability and strong infrastructures are most attractive. There are many “hybrid” type practice environments that can and should be investigated, including private practice settings that offer academic involvement, teaching opportunities, and resident interactions, as well as practices that have partnered with hospital or healthcare systems to assist with onboarding and employment. Direct employment through a viable healthcare system has become an increasingly popular option. However, even these job settings were forced to reduce physician reimbursement and benefits during the pandemic.
Word of mouth may be the most valuable strategy. Connect with former residents, attendings, and mentors as well as former medical friends and colleagues for job openings. Reach out even when practices may not be obviously advertising for positions as their postings may have been on sites outside your radar. Social media has certainly streamlined this type of inquiry.
For the employer, most will pursue traditional recruitment avenues, job boards, etc. Personal contacts and word of mouth continue to be highly effective strategies. Reach out to former residents, medical students, attendings, and colleagues to inquire about candidates that may be seeking employment. Be flexible about creating a harmonious job description that meets the needs and expectations of the applicant, which provides appropriate workload and opportunities and offers pathways for partnership, mentorship, and local, state, and national leadership. For those that cannot find a resident or fellow graduate, consider nonphysician options like advanced practice providers who can provide high-quality care, excellent collaborative relationships, and valuable practice promotion and coverage.
The challenges of COVID-19 have forced us all to modify our workflows and our approaches and foster creative changes and improvements that have strengthened our practices. These modifications will continue to be utilized along with other yet unidentified innovations as we emerge from the pandemic turmoil in the coming year. These adaptations can result in an improved future practice environment that will benefit all providers and shepherd the advancement and success of otolaryngologist-head and neck surgeons around the globe.
References
1. American Medical Association: COVID-19 Physician practice financial impact survey results. October 2020. www.ama-assn.org/system/files/2020-10/covid-19-physician-practice-financial-impact-survey-results.pdf