Clinical Practice Guideline: Nosebleed (Epistaxis)
“A nosebleed is a common occurrence, happening at some point in about six out of 10 people in the United States. Although it is common, methods of diagnosis and treatment for nosebleed have not been uniformly used across clinicians and settings.
Adapted from the 2020 Supplement to Otolaryngology–Head and Neck Surgery. Read the guideline at otojournal.org.
“A nosebleed is a common occurrence, happening at some point in about six out of 10 people in the United States. Although it is common, methods of diagnosis and treatment for nosebleed have not been uniformly used across clinicians and settings. To address that and to help reduce variations in care, this guideline provides evidence-based recommendations to improve quality of care,” said David E. Tunkel, MD, Chair of the guideline development group (GDG). Samantha Anne, MD, MS, and Spencer C. Payne, MD, served as assistant chairs, and Stacey L. Ishman, MD, MPH, and Richard M. Rosenfeld, MD, MPH, MBA, served as methodologists.
The overarching aim of this multidisciplinary guideline is to identify quality improvement opportunities in the management of nosebleed and to create clear, actionable recommendations for clinical practice.
This guideline is intended to promote best practices, reduce unjustified variations in care of patients with nosebleed, improve health outcomes, and minimize the potential harms of nosebleed and/or interventions to treat nosebleed.
“This is the first multidisciplinary, evidence-based guideline on nosebleed developed in the United States,” said Dr. Tunkel. “It informs clinicians about the current level of evidence and includes areas of improvement of practice—such as providing patient instructions for nasal packing care—that were developed by the guideline panel after a review of all the literature.”
This guideline discusses first-line treatments, such as nasal compression, application of vasoconstrictors, nasal packing, and nasal cautery. It also addresses more complex epistaxis management, which includes the use of endoscopic arterial ligation and interventional radiology procedures. Because the GDG recognized an opportunity for improved care, management options for two special groups of patients—patients with hereditary hemorrhagic telangiectasia (HHT) and patients taking medications that inhibit coagulation and/or platelet functions—are included.
This guideline does not apply to patients who have a previously diagnosed bleeding disorder, tumors of the nose or nasopharynx, vascular malformations of the head and neck, a history of recent facial trauma, or have undergone nasal and/or sinus surgery in the past 30 days.
Guideline Key Action Statements (KAS)
KAS1: Prompt management (recommendation)
At the time of initial contact, the clinician should distinguish the nosebleed patient who requires prompt management from the patient who does not.
KAS2: Nasal compression (recommendation)
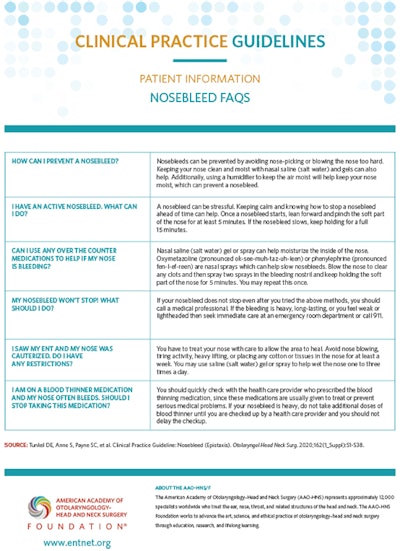
The clinician should treat active bleeding for patients in need of prompt management with firm, sustained compression to the lower third of the nose, with or without the assistance of the patient or caregiver, for five minutes or longer.
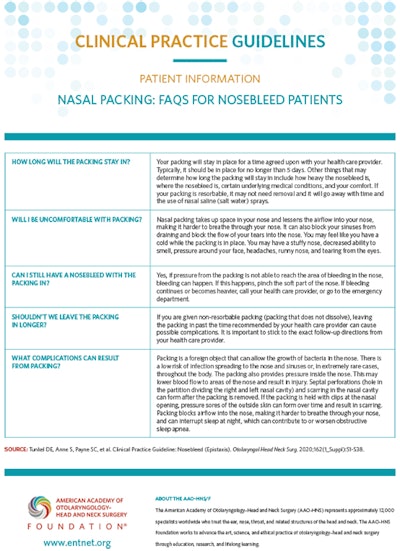
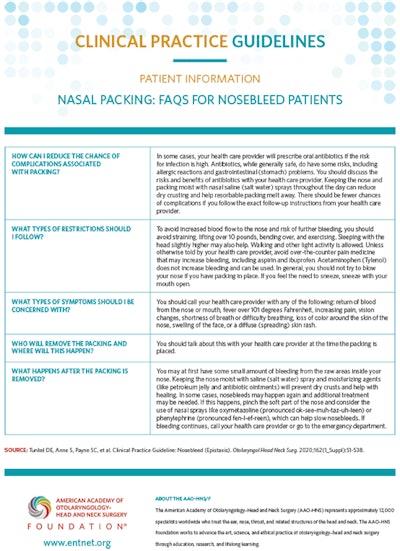
KAS3a: Nasal packing (recommendation)
For patients in whom bleeding precludes identification of a bleeding site despite nasal compression, the clinician should treat ongoing active bleeding with nasal packing.
KAS3b: Nasal packing in patients with suspected increased bleeding risk (recommendation)
The clinician should use resorbable packing for patients with a suspected bleeding disorder or for patients who are using anticoagulation or antiplatelet medications.
KAS4: Nasal packing education (recommendation)
The clinician should educate the patient who undergoes nasal packing about the type of packing placed, timing of and plan for removal of packing (if not resorbable), post-procedure care, and any signs or symptoms that would warrant prompt reassessment.
KAS5: Risk factors (recommendation)
The clinician should document factors that increase the frequency or severity of bleeding for any patient with a nosebleed, including personal or family history of bleeding disorders, use of anticoagulant or antiplatelet medications, or intranasal drug use.
KAS6: Anterior rhinoscopy to identify location of bleeding (recommendation)
The clinician should perform anterior rhinoscopy to identify a source of bleeding after removal of any blood clot (if present) for patients with nosebleeds.
KAS7a: Examination using nasal endoscopy (recommendation)
The clinician should perform, or should refer to a clinician who can perform, nasal endoscopy to identify the site of bleeding and guide further management in patients with recurrent nasal bleeding, despite prior treatment with packing or cautery, or with recurrent unilateral nasal bleeding.
KAS7b: Examination of nasal cavity and nasopharynx using nasal endoscopy (option)
The clinician may perform, or may refer to a clinician who can perform, nasal endoscopy to examine the nasal cavity and nasopharynx in patients with epistaxis that is difficult to control or when there is concern for unrecognized pathology contributing to epistaxis.
KAS8: Appropriate interventions for identified bleeding site (recommendation)
The clinician should treat patients with an identified site of bleeding with an appropriate intervention, which may include one or more of the following: topical vasoconstrictors, nasal cautery, and moisturizing or lubricating agents.
KAS9: Nasal cautery (recommendation)
When nasal cautery is chosen for treatment, the clinician should anesthetize the bleeding site and restrict application of cautery only to the active or suspected site(s) of bleeding.
KAS10: Ligation and/or embolization for persistent nosebleeds (recommendation)
The clinician should evaluate, or refer to a clinician who can evaluate, candidacy for surgical arterial ligation or endovascular embolization for patients with persistent or recurrent bleeding not controlled by packing or nasal cauterization.
KAS11: Management of patients using anticoagulation and antiplatelet medications (recommendation)
In the absence of life-threatening bleeding, the clinician should initiate first-line treatments prior to transfusion, reversal of anticoagulation, or withdrawal of anticoagulation/antiplatelet medications for patients using these medications.
KAS12: HHT identification (recommendation)
The clinician should assess, or refer to a specialist who can assess, the presence of nasal telangiectasias and/or oral mucosal telangiectasias in patients who have a history of recurrent bilateral nosebleeds or a family history of recurrent nosebleeds to diagnose hereditary hemorrhagic telangiectasia syndrome (HHT).
KAS13: Patient education and prevention (recommendation)
The clinician should educate patients with nosebleeds and their caregivers about preventive measures for nosebleeds, home treatment for nosebleeds, and indications to seek additional medical care.
KAS14: Nosebleed outcomes (recommendation)
The clinician or designee should document the outcome of intervention within 30 days or document transition of care in patients who had a nosebleed treated with non-resorbable packing, surgery, or arterial ligation/embolization.
The GDG included representatives from the fields of nursing, family medicine, emergency medicine, otolaryngology-head and neck surgery, pediatrics, rhinology, radiology, internal medicine, and hematology. The GDG also included a consumer/patient representative.
This guideline is intended for clinicians who evaluate and treat patients with nosebleed. This includes primary care providers such as family medicine physicians, internists, physician assistants, nurse practitioners, and pediatricians. It also includes specialists such as emergency medicine providers, otolaryngologists, interventional radiologists/neuroradiologists and neurointerventionalists, hematologists, and cardiologists. The target patient for the guideline is any individual aged three years and older with a nosebleed or history of nosebleed.
The nosebleed guideline was created using the methods listed in the AAO-HNSF “Clinical Practice Guideline Development Manual, Third Edition.” (https://journals.sagepub.com/doi/full/10.1177/0194599812467004)
Accompanying Resources:
- Plain Language Summary
- Executive Summary
- Slide deck
- Podcasts
- Patient handouts (in both English and Spanish)
- Official quick-reference pocket guide and app
Access all these resources and more at www.entnet.org/CPGNosebleed
The full guideline and other resources are available at www.entnet.org/CPGNosebleed and in Otolaryngology–Head and Neck Surgery as published at otojournal.org.
Guideline authors:
David E. Tunkel, MD (Chair), Samantha Anne, MD, MS (Assistant Chair), Spencer C. Payne, MD (Assistant Chair), Stacey L. Ishman, MD, MPH (Methodologist), Richard M. Rosenfeld, MD, MPH, MBA (Methodologist), Peter J. Abramson, MD, Jacqueline D. Alikhaani, Margo McKenna Benoit, MD, Rachel S. Bercovitz, MD, MS, Michael D. Brown, MD, MSc, Boris Chernobilsky, MD, David A. Feldstein, MD, Jesse M. Hackell, MD, Eric H. Holbrook, MD, Sarah M. Holdsworth, MSN, APRN, Kenneth W. Lin, MD, MPH, Meredith Merz Lind, MD, David M. Poetker, MD, MA, Charles A. Riley, MD, John S. Schneider, MD, MA, Michael D. Seidman, MD, Venu Vadlamudi, MD, Tulio A. Valdez, MD, Lorraine C. Nnacheta, MPH, DrPH, Taskin M. Monjur
Endorsements:
The guideline is endorsed by the American College of Emergency Physicians (ACEP), American College of Radiology (ACR), American Rhinologic Society (ARS), American Society of Hematology (ASH), American Society of Pediatric Otolaryngology (ASPO), Cure Hereditary Hemorrhagic Telangiectasia (Cure HHT), Society of Interventional Radiology (SIR), Society of Neurointerventional Surgery (SNIS), Society of Otorhinolaryngology and Head-Neck Nurses (SOHN), and The Triological Society.
Affirmation of Value:
“The American Geriatrics Society (AGS) affirms the value of this document. Affirmation of value means that AGS supports the general principles in this document and believes it is of general benefit to its membership.”
Disclaimer:
This guideline is intended to focus on evidence-based quality improvement opportunities judged most important by the working group. It is not intended to be a comprehensive, general guide for managing patients with nosebleed. In this context, the purpose is to define useful actions for clinicians, generalists, and specialists from a variety of disciplines to improve quality of care. Conversely, the statements in this guideline are not intended to limit or restrict care provided by clinicians based upon their experience and assessment of individual patients.