Coding Update: New CMS G-Code/Modifier Requirements for Therapy Services
Michael Setzen, MD Immediate-Past Coordinator for Practice Affairs; Manderly Cohen, MS CCC-SLP, and Jenna Minton, Esq., Senior Manager of Health Policy For CY 2013, CMS finalized several key changes to reporting requirements associated with the provision of therapy services, and beginning on January 1, 2013, it implemented a claims-based data collection strategy to collect data on patient function. This policy encompassed a wide array of therapy services, including the Medicare Part B outpatient therapy benefit, therapy services under the Comprehensive Outpatient Rehabilitation Facility (CORF) benefit, and “incident to” services furnished by physicians or nonphysician practitioners, and included services furnished in hospitals, critical access hospitals (CAHs), skilled nursing facilities (SNFs), CORFs, rehabilitation agencies, home health agencies (when the beneficiary is not under a home health plan of care), and private offices. CMS defines the term “therapists” as all practitioners who furnish outpatient therapy services, including physical therapists, occupational therapists, and speech-language pathologists in private practice and those therapists who furnish services in the institutional settings, physicians, and nonphysician practitioners (including physician assistants, nurse practitioners, and clinical nurse specialists, as applicable). Under this policy, claims for therapy services must now include non-payable G-codes and modifiers, which will allow the agency to capture data on the beneficiary’s functional limitations at various points during the provision of therapy. For therapy services being furnished that are not intended to treat a functional limitation, the therapist should use the G-code for “other” and the modifier representing zero. A specific example of how this would apply in otolaryngology is when performing FEES/FEESST or providing therapy, including speech-language evaluation and treatment services for Medicare Part B beneficiaries, providers must report outcomes on claim forms. To facilitate this reporting, CMS established non-payable G-codes for reporting on claims for Medicare Part B beneficiaries receiving therapy services. Each non-payable G-code listed on the claim form must be accompanied with a severity/complexity modifier. The modifier represents the functional impairment on a 7-point severity/complexity scale. G Codes When billing FEES/FEESST CPT codes, specifically 92610 Evaluation of oral and pharyngeal swallowing function, 92612 Flexible fiberoptic endoscopic evaluation of swallowing by cine or video recording, and 92616 Flexible fiberoptic endoscopic evaluation of swallowing and laryngeal sensory testing by cine or video recording, where only an evaluation was performed and the patient will not be seen for therapy at the same facility, all three swallowing G-codes must be used when billing for the evaluation (G8996, G8997, and G8998) in addition to the appropriate severity modifier for each code. Click here for a full list of available G-codes for reporting therapy services. Severity Modifiers Note: Corresponding National Outcomes Measurement System (NOMS) Functional Communication Measures [PDF] levels are listed here. Use of NOMS can assist with G-code and severity modifier selection, but is not required by CMS. Members seeking additional information can access a full summary of this issue at http://www.entnet.org/Practice/CMS-News.cfm.
Michael Setzen, MD
Immediate-Past Coordinator for Practice Affairs;
Manderly Cohen, MS CCC-SLP, and Jenna Minton, Esq., Senior Manager of Health Policy
For CY 2013, CMS finalized several key changes to reporting requirements associated with the provision of therapy services, and beginning on January 1, 2013, it implemented a claims-based data collection strategy to collect data on patient function. This policy encompassed a wide array of therapy services, including the Medicare Part B outpatient therapy benefit, therapy services under the Comprehensive Outpatient Rehabilitation Facility (CORF) benefit, and “incident to” services furnished by physicians or nonphysician practitioners, and included services furnished in hospitals, critical access hospitals (CAHs), skilled nursing facilities (SNFs), CORFs, rehabilitation agencies, home health agencies (when the beneficiary is not under a home health plan of care), and private offices.
CMS defines the term “therapists” as all practitioners who furnish outpatient therapy services, including physical therapists, occupational therapists, and speech-language pathologists in private practice and those therapists who furnish services in the institutional settings, physicians, and nonphysician practitioners (including physician assistants, nurse practitioners, and clinical nurse specialists, as applicable). Under this policy, claims for therapy services must now include non-payable G-codes and modifiers, which will allow the agency to capture data on the beneficiary’s functional limitations at various points during the provision of therapy. For therapy services being furnished that are not intended to treat a functional limitation, the therapist should use the G-code for “other” and the modifier representing zero.
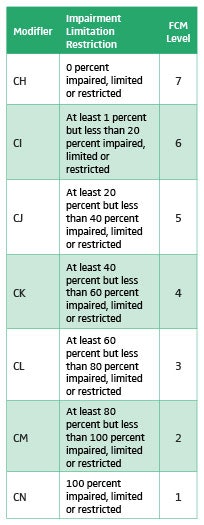
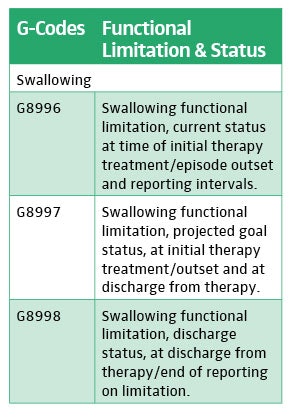
A specific example of how this would apply in otolaryngology is when performing FEES/FEESST or providing therapy, including speech-language evaluation and treatment services for Medicare Part B beneficiaries, providers must report outcomes on claim forms. To facilitate this reporting, CMS established non-payable G-codes for reporting on claims for Medicare Part B beneficiaries receiving therapy services. Each non-payable G-code listed on the claim form must be accompanied with a severity/complexity modifier. The modifier represents the functional impairment on a 7-point severity/complexity scale.
G Codes
When billing FEES/FEESST CPT codes, specifically 92610 Evaluation of oral and pharyngeal swallowing function, 92612 Flexible fiberoptic endoscopic evaluation of swallowing by cine or video recording, and 92616 Flexible fiberoptic endoscopic evaluation of swallowing and laryngeal sensory testing by cine or video recording, where only an evaluation was performed and the patient will not be seen for therapy at the same facility, all three swallowing G-codes must be used when billing for the evaluation (G8996, G8997, and G8998) in addition to the appropriate severity modifier for each code.
Click here for a full list of available G-codes for reporting therapy services.
Severity Modifiers
Note: Corresponding National Outcomes Measurement System (NOMS) Functional Communication Measures [PDF] levels are listed here. Use of NOMS can assist with G-code and severity modifier selection, but is not required by CMS.
Members seeking additional information can access a full summary of this issue at http://www.entnet.org/Practice/CMS-News.cfm.